The highly anticipated final overall survival (OS) results from the phase III FLAURA2 trial demonstrate that first-line osimertinib plus chemotherapy significantly improves overall survival (OS) compared with osimertinib monotherapy for patients with EGFR-mutated (EGFRm) advanced non-small cell lung cancer (NSCLC).
So said David Planchard, MD, PhD, who presented the findings during the first of two Presidential Symposia at the 2025 World Conference on Lung Cancer.
“These compelling OS results confirm osimertinib plus chemotherapy as a first-line standard of care for this patient population,” said Dr. Planchard, a thoracic oncologist and Head of the Thoracic Pathology Committee at Gustave Roussy, Villejuif, France, and President of the International Center for Thoracic Cancers.
Study Background and Design
Osimertinib, a third-generation, CNS-active EGFR-TKI, is currently a preferred first-line treatment for EGFRm advanced NSCLC.
The global, open-label, randomized trial enrolled 557 patients with previously untreated, EGFRm locally advanced or metastatic NSCLC.
Participants were randomized 1:1 to receive either osimertinib plus chemotherapy or osimertinib monotherapy. Patients received 80 mg osimertinib once daily alone until disease progression/discontinuation criteria or with pemetrexed with cisplatin or carboplatin every 3 weeks for four cycles, followed by maintenance therapy. The primary endpoint was progression-free survival (PFS); OS was a key secondary endpoint.
Key Results
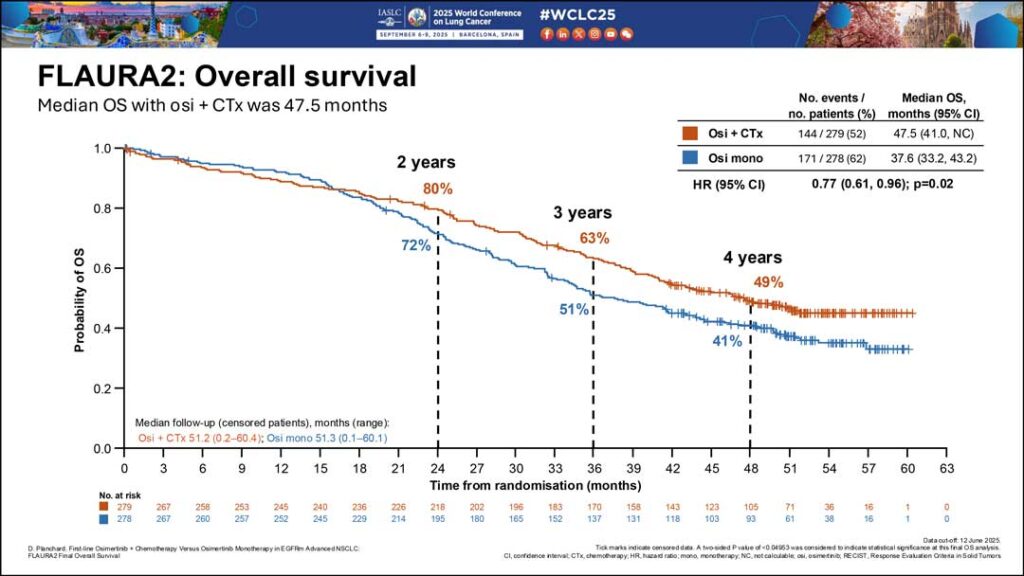
Osimertinib combined with chemotherapy demonstrated a statistically significant and clinically meaningful improvement in OS versus osimertinib monotherapy (median OS: 47.5 vs. 37.6 months, respectively; HR 0.77) at a median follow-up of approximately 57% maturity, which translates to 51.2 and 51.3 months, respectively.
Dr. Planchard said this is the longest OS in the global space, and the OS benefit was observed regardless of the predefined subgroup population. The 36-month survival rates were 63% compared with 51%.
“The median OS of patients who received osimertinib plus chemotherapy was significantly prolonged compared to osimertinib monotherapy,” Dr. Planchard said. “The osimertinib monotherapy performed as expected, and the median OS of osimertinib is comparable to what has already been presented in the FLAURA trial.”
The osimertinib-chemotherapy combination maintained a manageable safety profile consistent with the known toxicities of the individual treatments, with no new safety signals identified at longer follow-up.
The duration of exposure to osimertinib was prolonged (30.5 months) in the combination arm, compared with the monotherapy arm (21.2 months). The duration of exposure to pemetrexed was 8.3 months in the combination arm, Dr. Planchard noted.
An OS benefit was observed in the combination arm despite 77% of patients in the standard-of-care arm receiving second-line therapy, 72% of which was platinum-based chemotherapy. In the osimertinib plus chemotherapy arm, 69% of patients who experienced disease progression received a subsequent line of treatment. The most common lines of treatment in the combination arm were platinum-based chemotherapy (44%) and non-platinum-based chemotherapy (30%).
No additional treatment-related deaths were observed in the osimertinib-plus-chemotherapy arm, while one occurred in the osimertinib-monotherapy arm. Adverse events leading to osimertinib discontinuation remained low in the combination arm (12%) compared to the monotherapy arm (7%).
Future Implications
Based on the final OS results from the FLAURA2 study, the addition of chemotherapy provides a meaningful survival advantage for patients with EGFRm advanced NSCLC. Additionally, the combination treatment was associated with a longer duration of exposure to osimertinib and a manageable safety profile.
“So, with this, we can conclude first-line osimertinib with chemotherapy demonstrates [superiority over] osimertinib monotherapy,” Dr. Planchard said.