Thoracic oncology care providers have been dealing with the on-target dermatologic effects of EGFR-targeted agents for at least 20 years. As therapies have evolved, so too have the best practices for management of dermatologic toxicities. Now, another shift—one toward a patient-first prophylactic approach to these effects–is taking place. The randomized phase II COCOON trial, interim data for which was presented at the 2025 European Lung Cancer Congress (ELCC), outlined an easily accessible prophylactic regimen for use with amivantamab plus lazertinib in the first line for patients with EGFR-mutated locally advanced or metastatic NSCLC.1 As Martin Dietrich, MD, PhD, explains in the following Q&A, use of the regimen was found to reduce both the incidence and severity of dermatologic events involving the skin, scalp, and nails. Alyson Singer, APRN, OCN, reviews best practices for provision of patient education about the side effects and the prophylactic regimen.
Martin F. Dietrich, MD, PhD, is a hematologist/oncologist within the US Oncology Network and an Assistant Professor of Internal Medicine at the University of Central Florida in Orlando. Dr. Dietrich has a special research interest in treatment of thoracic malignancies and diagnostic approaches to the disease. He is a principal investigator at Sarah Cannon Research Institute for a number of precision medicine-based trials and a member of the IASLC, among other organizations.
Please provide some background regarding the on-target dermatologic side effects (ie, skin rash, scalp rash, and nail effects) associated with amivantamab plus lazertinib. What do we know about how the rash affects quality of life?

In the MARIPOSA study, a first-line combination trial of amivantamab and lazertinib for EGFR-mutated non-small cell lung cancer, dual targeting of the EGFR receptor, produced noteworthy on-target side effects,2 which can affect any of the outer surfaces of the body including some of the more difficult areas of the skin such as the nail beds, scalp, and intertriginous areas. These on-target effects can clinically display as dermatitis/rash of skin and scalp and paronychia, an issue of particular concern. Effects can be very mild, presenting with a slight redness and some irritation, or they can be more significant and display as more acne-like eruptions. Effects can even be more severe, with blistering formation and desquamation. We can also see similar on-target effects on the inner surfaces of the oral mucosa and the gastrointestinal tract, which is more common but these can also occur on the outer linings of both as well. Amivantimab targets the extracellular domain of the EGF receptor, consequently it does not distinguish between wild-type and mutated receptor where mutations happen in the intracellular kinase domain. Dermatologic eruption is, therefore, a frequent occurrence. MARIPOSA data showed that 68% of patients developed paronychia, with 11% of those grade 3 or higher, and 62% developed rash, with 15% of grade 3 or higher. Dermatitis acneiform was seen in 29% of patients, and 8% of those had grade 3 or higher, but there were very low rates of grade 3 or higher stomatitis and pruritus.2
Quality-of-life impact obviously is significantly different depending on severity. I think there is also a difference between how men and women perceive the low-grade mostly cosmetic concerns. But there can be more significant quality-of-life impairment with pruritus, which can result in discomfort, superinfections, and also functional impairment based on a combination of these side effects.

These results show that the enhanced-care protocol really should be treated as the standard of care when using amivantamab, whether alone or in combination.
Martin F. Dietrich, MD, PhD
Why is it important to treat prophylactically versus reactively?
The COCOON trial was a clinical study evaluating a prophylactic regimen versus standard-of-care skin care approach for use with amivantamab. The trial built on the experience of MARIPOSA and MARIPOSA-2 and incorporated multiple skin protective interventions including oral and topical antibiotics, chlorhexidine treatments for the nail and nailbeds, and general skin moisturization.1 It is important to remember that the first-generation EGFR antibodies that we have been using in clinics, such as cetuximab and panitumumab, have been used with a prophylactic approach to these on-target effects for a long time, so this is not a novel concept, but it is one that we are reapplying to amivantamab, alone and in combination with lazertinib. The prophylactic enhanced-care protocol in COCOON was adapted using previous experiences and from corresponding guidelines. The trial used the MARIPOSA treatment regimen with either standard-of-care dermatologic management or with enhanced dermatologic management, which included three pillars of treatment. The first pillar was prophylactic antibiotics, which included a tetracycline for the first 12 weeks, either oral doxycycline or minocycline, followed by topical clindamycin for the remainder of the year on the scalp daily before bedtime. A prophylactic protocol for paronychia and paronychia super infection used chlorhexidine 4% on the fingernails and toenails every day, and a prophylactic skin moisturization and treatment protocol required a ceramide-based moisturizer on the body and face at least daily using La Roche Posay Lipikar AP+M Repair Moisturizer. So this is the enhanced-care protocol in the study, and the idea was to initiate this prior to the start of treatment to essentially mitigate these side effects.
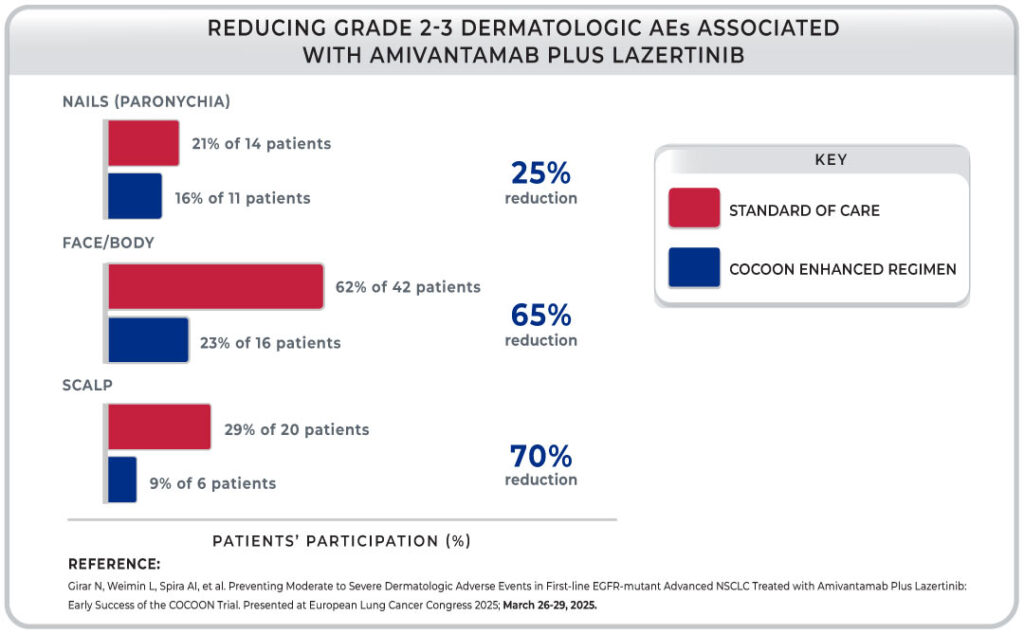
There was a significant drop in the dermatologic side effects using both the standard-of-care and enhanced approaches, but the enhanced protocol resulted in a 50% reduction in the incidence of grade 2 or greater dermatologic adverse events by week 12, with only 39% of patients experiencing these compared with 76% of patients who received standard of care. Of that 76%, 8.8% experienced grade 3 or greater effects, but only 4% of patients on the enhanced protocol had high-grade effects. So that is of substantial importance. I do want to highlight the protection of the scalp. There was a three-fold reduction in the number of reported adverse events of grade 2 or greater with standard of care versus enhanced care with the COCOON protocol.1 In my practice, we often add topical shampoos with beclomethasone for management of scalp-related rashes that can be particularly challenging.
These results show that the enhanced-care protocol really should be treated as the standard of care when using amivantamab, whether alone or in combination.
How will the results from the COCOON trial impact your daily patient care?
Use of prophylactic interventions for EGFR on-target antibody-related dermatologic effects is pretty standard management. One of the issues that we have with the third-generation EGFR targeted therapies in lung cancer is that we have unlearned the use of prophylactic interventions because the newer, third-generation EGFR TKIs are largely mutation specific wild-type sparing.
This is not the case for amivantamab, which targets the extracellular domain and, therefore, does not differentiate between cancer-resident and normal-tissue EGFR receptors. Therefore, it is expected to see these on-target effects again in practice. This is a trade off with the significantly improved efficacy of the combination. We have all learned our tips and tricks about how best to implement a protective regimen for skin, nails, and scalp, and the COCOON enhanced approach makes the prophylactic regimen manageable, for both us and the patients, as well as effective.

These results show that the enhanced-care protocol really should be treated as the standard of care when using amivantamab, whether alone or in combination.
Martin F. Dietrich, MD, PhD
I believe it is very important that, for general oncology providers who are treating patients with anti-EGFR antibodies in colon cancer or head and neck cancer, for example, to be very well versed in this prophylactic regimen and for them to routinely implement this prior to starting of anti-EGFR therapies. Typically, as thoracic oncology subspecialty providers, we were able to get away with a little less in terms of treatment for dermatologic side effects because the third-generation EGFR inhibitors simply did not require routine prophylaxis. With the improved efficacy for amivantamab plus lazertinib in MARIPOSA,2 the utility and necessity of this enhanced skin care protocol becomes very clear.
Alyson Singer, APRN, OCN is a hematology/oncology nurse practitioner at US Oncology. Her professional focus includes patient education, symptom management, and supportive care for patients undergoing treatment. Ms. Singer has a particular interest in the prevention and management of treatment-related side effects, including dermatologic toxicities, and is passionate about empowering patients with strategies to improve quality of life throughout the cancer care continuum.
Please discuss some of the quality-of-life issues that can be associated with dermatologic events from EGFR-related therapies.

Building off of what Dr. Dietrich said, the dermatologic events that we see with these drugs can have a pretty profound impact on the patient’s quality of life. Depending on the severity of the rash, a patient may experience emotional distress too because they feel like people might be looking at them differently. This is even truer when the rash is more visible, on the face, or if it is painful. Patients may experience problems with sleep and social anxiety. Even if the rash is mild, the persistent symptoms can become a reminder of the disease itself. Patients want to have hope and stay positive as they go through therapy, but sometimes that is difficult to do when they are reminded of their diagnoses every time they look in the mirror. This can also lead to decreased adherence in the long run if the patients begin to feel discouraged or overwhelmed, which is why early and proactive intervention is key to treatment adherence and, obviously, to the patient’s well-being and quality of life.
How do you ensure proactive communication about potential dermatologic side effects and their mitigation during patient visits?
I can say that, in our practice, we have already shifted toward prophylactic management of dermatologic side effects, as outlined in the COCOON trial. We want to keep the patients on treatment and make sure that their quality of life stays high. I think the most important part of this is proactive communication with the patient and early provision of patient education. I tell patients upfront that we are going to start these prophylactic medications to hopefully reduce the effects of treatment, which should help maintain their quality of life. As an advanced practitioner, your exposure to the patient is limited, so I instruct patients to please let me know right away if they notice any skin, scalp, or nail changes. The whole conversation is very candid and focuses on what effects could happen, how we are already working to prevent them, and the importance of timely communication if prevention does not work. I think it is important for us to really stress that patients should call us between appointments or contact us in the portal, as necessary. Photos can be helpful, both for patients — who may or may not notice slow, progressive changes — and for healthcare providers, to help assess severity and tailor management.

I can say that, in our practice, we have already shifted toward prophylactic management of dermatologic side effects, as outlined in the COCOON trial. We want to keep the patients on treatment and make sure that their quality of life stays high.
Alyson Singer, APRN, OCN
What are your preferred methods of educating patients and caregivers about symptom reporting?
Education is key in my world, and I really try to make sure that patients know what to expect and they feel empowered in their own care. I think having a “brown bag” visit to review all of the patient’s current skin care and hygiene products is a great thing to do. These visits may take a little more time, but they are necessary because patients may be following advice they got online or from a friend when entering treatment, and that advice could actually be hurting them versus helping to prevent a side effect.
I prefer to send the patients home with as much material as I can. Thinking back to when I was in school, I definitely did not remember every word that was said during an hour-long lecture, so I think it is important for the patients to go home with clear, digestible, written materials they can refer to while they are on treatment. Also, caregivers are not always able to attend every appointment, so it is important for them to have resources about the timeline and what to expect so that unexpected events are more of a focus.

Education is key in my world, and I really try to make sure that patients know what to expect and they feel empowered in their own care.
Alyson Singer, APRN, OCN
It can be overwhelming, especially when you have this rash and you do not know what is normal or not, so I try to give patients as much printed information as I can. I use resources from specialty societies and advocacy organizations. If the patient is a little more tech savvy, I will give them the link to the therapy’s website because those sites often include visuals and timelines to help patients recognize what is normal and when to reach out.
When prophylactic approaches fail, how do you manage more complex cases in the community setting where oncodermatologists may not be a resource and/or wait time for patients may be excessive?
Because we do try to refer out as seldom as possible and because it can be difficult for the patient to be seen in a timely manner, we rely heavily on protocols like that in COCOON to bridge that gap. When using the enhanced prophylactic regimen, we have seen a meaningful reduction in the number of cases requiring specialty referral. For the complex cases, we try to collaborate with general dermatologists in our network, and we have made connections with specific dermatologists over time who are used to seeing the effects associated with EGFR inhibition. For new dermatology partners, we’re happy to share literature and clinical photos to guide treatment decisions. We try not to rush to discontinue the cancer therapy due to toxicity unless it is absolutely necessary, but if symptoms progress despite prophylactic approaches and standard management strategies, our first step is to optimize the treatment locally and try to consult the dermatologist in the area. We have got really great front desk staff here who will try to call around to as many practices as necessary to get the patient seen as early as possible. That said, the need for referrals has decreased significantly since we implemented a proactive, COCOON-informed approach.
References
- 1. Girar N, Weimin L, Spira AI, et al. Preventing Moderate to Severe Dermatologic Adverse Events in First-line EGFR-mutant Advanced NSCLC Treated with Amivantamab Plus Lazertinib: Early Success of the COCOON Trial. Presented at European Lung Cancer Congress 2025; March 26-29, 2025.
- 2. Cho BC, Lu S, Felip E, et al. Amivantamab plus Lazertinib in Previously Untreated EGFR-Mutated Advanced NSCLC. N Engl J Med. 2024;391:1486-1498.