Using LDCT to Boost Lung Cancer Prevention Strategies: A Pro/Con
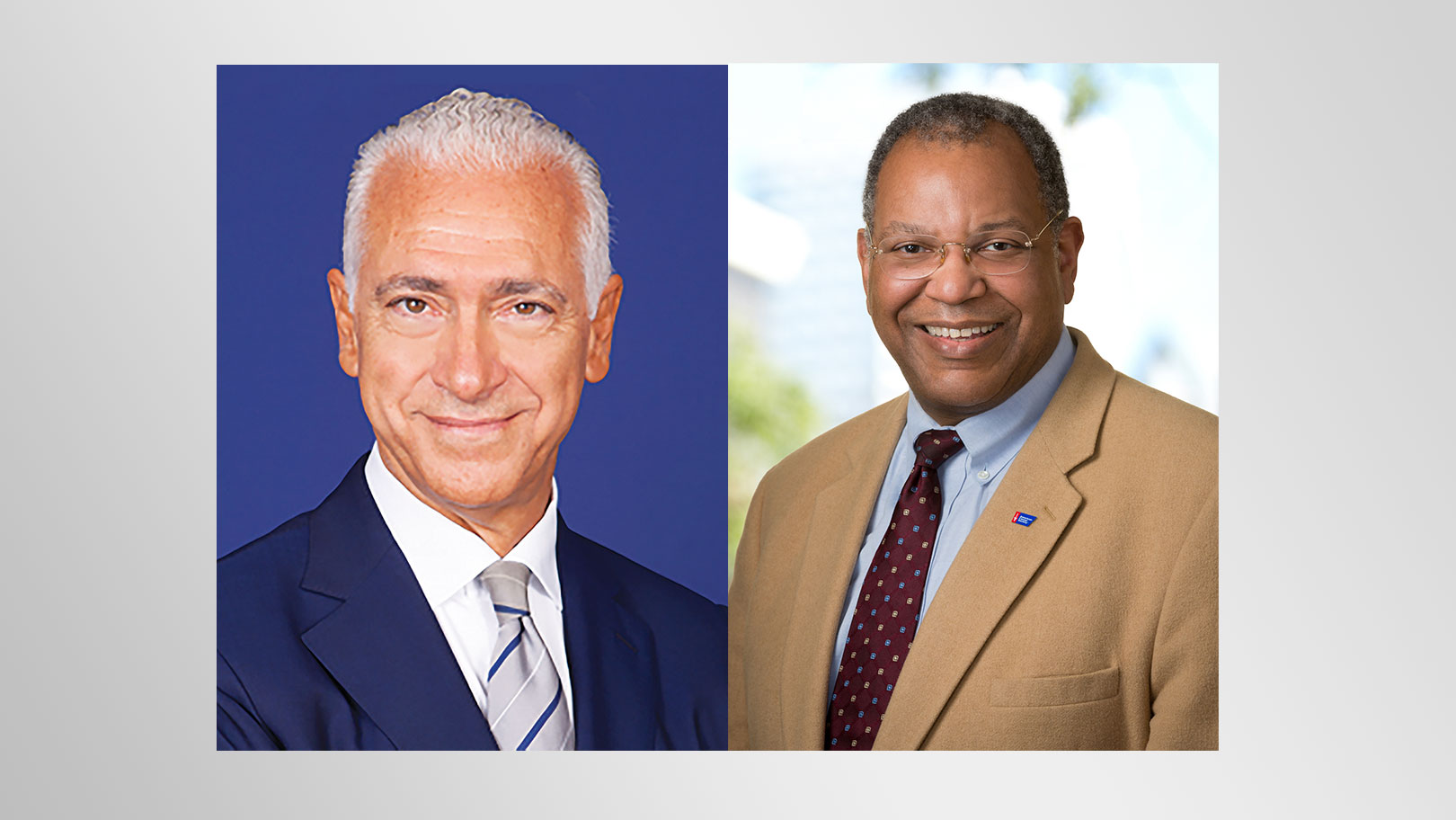
By Ugo Pastorino, MD
Now we know from robust randomized trials that systematic screening with low-dose computed tomography (LDCT) of the chest can reduce lung cancer mortality in heavy smokers by increasing the proportion of cases detected in an early stage,1,2 when they are amenable to curative surgery with minimally invasive procedures. On the whole, prospective studies suggest that the magnitude of benefits can increase with longer screening periods,3 which is understandable given the continuous increase of lung cancer risk with age.
We also know that double-source ultra LDCT scanners can further minimize the total radiation exposure of a 20-year screening program, with very low cumulative radiation risk. New technologic developments can guarantee very high diagnostic standards through the validation of automatic reading software, which cuts the time and cost of early detection and makes LDCT screening applicable to millions of people.
In every large-scale cancer screening program, such as in breast or prostate cancers, there is a non-negligible probability of treating asymptomatic individuals with indolent disease, who would have never suffered from cancer consequences without such anticipated detection. However, 20 years of LDCT research has taught us that active surveillance of non-solid or sub-solid pulmonary lesions can help us avoid the large majority of unnecessary resections for indolent or slow-growing cancers without compromising screening efficacy.4 On the contrary, individuals with non-solid or sub-solid lesions have shown a greater risk of invasive lung cancer in other sites of their lungs and require monitoring by annual LDCT for many years. Even though the experience accumulated by prospective trials in selected centers of excellence may be difficult to implement in every general hospital, prevention of overtreatment has proven feasible and represents a primary goal in LDCT screening.
So why then we don’t see a growing demand and advocacy groups clamoring for LDCT screening facilities, as we have seen for mammographic screening many years ago? This is mainly because life-long smokers and their physicians ignore or don’t trust the results of screening trials. High-risk individuals and doctors share a dominant nihilism about lung cancer outcomes and fear of potential harms from unnecessary surgery. They are convinced that after many years of smoking, the damage is done, and living or dying is only a matter of chance. There is a dose of reality in such skepticism, as large-scale cohort studies in the United States have demonstrated that only 20% of current and 10% of former smokers die of lung cancer.5 In fact, the major causes of death for this group, such as cardiovascular diseases, chronic obstructive pulmonary disease, and other cancers, are unlikely to be modified by LDCT screening itself.
We have not yet been able to convey the message that besides lung cancer diagnosis, LDCT provides relevant information on a smoker’s level of cardio-pulmonary damage at that time in his or her life. Data such as type, site, and extent of emphysema, lung inspiratory and expiratory volumes, bronchial thickening, size of thoracic vessels, and calcium scoring of each coronary artery and aorta could be used to reduce the global risk of death through targeted chemoprevention. A number of risk-assessing models have been applied to improve the selection to LDCT screening, but even the best-performing tools, such as PLCO12 (Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial),6 can only catch 60% of future lung cancers. Rather than choosing if a subject is “in or out” CT screening eligibility for the entire life, we have now the option of modulating the long-term screening schedule on the basis of initial LDCT, to define the individual risk profile and adopt a personalized screening plan. Unlike mammographic screening, which has offered the same program to every woman for decades, LDCT screening can be individually tailored by adjusting duration and frequency on the basis of first LDCT examination.
Very few clinical studies have assessed the technical feasibility and utility of liquid biopsy to test blood biomarkers in the context of LDCT screening. Such a research effort will improve our knowledge on the interaction between tumor microenvironment, genomic field cancerization, and immunologic surveillance in lung carcinogenesis. Now the time has come to test their real value through randomized prospective trials measuring the global outcome of LDCT screening with or without blood biomarkers, in terms of differential diagnosis of indeterminate LDCT lesions, risk prediction, screening intensity, and total mortality reduction.
We should not forget that lung cancer is a preventable disease in more than 80% of cases, and we should never let down our guard against cigarette smoking. Offering LDCT screening as an alternative to primary prevention would be a real disaster, particularly in Europe and in the Far East, where the proportion of current smokers continues to grow. On the other hand, the damage profile acquired with baseline LDCT could be used to boost preventive strategies. I don’t particularly like the concept of a “teachable moment” with respect to LDCT screening; instead, I prefer the idea of “personalized therapy” of chronic addiction. There is already sufficient evidence that quitting during the screening period, with or without anti-tobacco drugs, can achieve a significant reduction of all-cause mortality. Even though many smokers who would be eligible for LDCT screening don’t want to quit, they may change their mind after their chest has been screened, if the whole team is giving the right information along with pharmacologic support.7
References:
- National Lung Screening Trial Research Team; Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409.
- de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med. 2020;382(6):503-513
- Pastorino U, Silva M, Sestini S, et al. Prolonged lung cancer screening reduced 10-year mortality in the MILD trial: new confirmation of lung cancer screening efficacy. Ann Oncol. 2019;30(7):1162-1169.
- Silva M, Prokop M, Jacobs C, et al. Long-Term Active Surveillance of Screening Detected Subsolid Nodules is a Safe Strategy to Reduce Overtreatment. J Thorac Oncol. 2018;13(10):1454-1463.
- Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368(4):351-364.
- Tammemagi MC, Katki HA, Hocking WG, et al. Selection criteria for lung-cancer screening. N Engl J Med 2013;368:728-736.
- Sands J, Milan MSD, Oxnard GR, et al. Lung Screening Benefits and Challenges: A Review of The Data and Outline for Implementation. J Thorac Oncol. Published November 11, 2020.
The Argument for Caution in Advocating Lung Cancer Screening: A U.S. Perspective (A Pro/Con)
By Otis W. Brawley, MD, MACP, FASCO, FACE
Although I am not against lung cancer screening, I do believe we should be cautious and circumspect in our advocacy and implementation of it. I think we must focus on all the anticancer interventions that are proven to save lives, and prioritize them. Having run a cancer center, I realize that resources are not infinite. In the United States, the most expensive healthcare system in the world, many hospitals are financially strapped. For most hospital systems, ramping up a lung cancer screening program and doing it right will mean depriving resources from other lifesaving services. Ironically, the hospitals and clinics that are most likely to curtail other lifesaving services to create a lung cancer screening service are those that take care of a high number of poor and minority patients. The lung cancer screening movement has the potential to increase cancer health disparities in the United States.
We are indeed fortunate that two prospective randomized studies1,2 demonstrate that a program of regular low-dose spiral CT screening, for persons at high risk for lung cancer, with high-quality diagnostics and treatment reduces the relative risk of death from lung cancer. Indeed, it is rare in medicine to have two large studies that so clearly agree. One model suggests that widespread, high-quality lung cancer screening in the United States could potentially prevent 12,000 lung cancer deaths per year.3
When lung cancer screening was first considered, it was viewed as the only opportunity to reduce mortality beyond primary prevention. In recent years, there have been exciting improvements in lung cancer management. We have entered an exciting new era in which diagnostic and treatment tools in addition to screening have moved forward from where we were more than a decade ago, when the National Lung Screening Trial was completed.1 These advances mean it is now possible to save even more lives from lung cancer.
Informing Patients About Both Benefits and Risks
It is not surprising to see advocacy groups enthusiastically embrace lung cancer screening. After all, some of these groups advocated lung cancer screening years before the definitive studies proved it saved lives. Today we have radio, television, and internet advertising, funded by advocacy groups, drug companies, device manufacturers, and hospitals, touting the value of lung cancer screening. A recent radio commercial funded by the American College of Radiology quotes several influential organizations as emphatically urging people to get screened for lung cancer. Interestingly, when I read the statements from those organizations, they recommend screening for those who have access to high-quality screening, diagnostics, and treatment and consent to it after being informed of the potential benefits and risks of screening, diagnosis, and treatment.
The failure of advocates to emphasize that candidates for screening should be told of the potential benefits and risks of screening, and be allowed to make an informed decision regarding screening, is a legitimate reason for patients to distrust those of us in medicine. This, combined with the failure to respect personal decisions to forego screening, lead many to fear seeking health care. It is a major cause of racial health disparities in the United States. I attribute this failure to respect the individual patient’s decision to enthusiasm for saving lives, but it does have an element of paternalism. When consenting is done right, 42% of screening candidates in the Veterans Health Administration system refused screening.4
We have data to show that implementing a lung cancer screening program is difficult and resource intensive and that even if done right, it can kill people. The National Lung Screening Trial was conducted in 30 of the finest hospitals in the United States. This trial randomly assigned more than 54,000 persons at high risk of lung cancer because of age and smoking history. After a decade of follow-up, it demonstrated that the group of approximately 27,000 people assigned to the low-dose spiral CT arm had approximately 85 to 90 fewer lung cancer deaths than the group of approximately 27,000 people assigned to the control arm. In the intervention arm, there were 16 deaths within 60 days of an invasive procedure that was caused by screening. One way of looking at this is that there were 5 to 6 lives saved per 1 life lost.1 This is an older population with a history of smoking. Some deaths are to be expected even among those treated in some of the finest hospitals in the United States. To my knowledge, the NELSON trial has not addressed the risks of screening.2
Defining ‘Doing It Right’
Now let us look at the real world. When implemented in the community, the emphasis is often only on screening and not on a long-term program of screening and care. Many centers have found it difficult to make certain that patients with suspicious or even proven lesions can be assured of getting the care they need. We cannot let screening be the sole focus, with an assumption of benefit. To realize the goal of saving more lives, we must wrap our arms around the entire process of lung cancer care. “Doing it right” means assuring high-quality care every step of the way. By the way, patterns of care studies show that a substantial proportion of Americans with lung cancer of all stages of disease have difficulty accessing adequate care.1 The treatment disparities are greatest for patients with early-stage lung cancer.5
As a physician who has run a cancer center and tried to provide good cancer care in the real world of U.S. medicine, perhaps my approach is tempered. I am not against lung cancer screening; I am against the overpromotion and overpromise of lung cancer screening at the cost of providing other lifesaving interventions.
Rather than continue to say what I am not against, perhaps I should say what I am for. I am for every hospital system administrator looking at their resources and figuring out what they can offer to their population, such that they prevent as many deaths as possible. In the case of lung cancer screening, I support it when one can afford the imaging equipment and employment of the multidisciplinary team needed to do it right. The team includes not just medical specialists such as diagnostic and interventional radiologists, pathologists, pulmonologists, medical oncologists, radiation oncologists, and thoracic surgeons but also nursing specialists and social workers.4 A screening program must offer all the supports necessary to guarantee the patient has access to all services from screening to diagnostic to treatment. The hospital choosing to offer lung cancer screening absolutely must have well-running breast and colon cancer screening and treatment services. In my opinion, these services have the potential of saving far more lives than a well-run lung cancer screening service.
Editor’s Note:
In Europe, for example, where lung cancer screening has been gradually implemented in a few countries, the scenario is quite different than that in the United States. Instead of common implementation in any interested institution, screening is started in high-volume centers and the multidisciplinary team has already been established. The idea of a central reading does allow for administration of LDCT in provincial institutions, but the final decisions and any invasive procedures are performed in the institution that runs all appropriate services.
References:
- National Lung Screening Trial Research Team; Aberle DR, Adams AM, Berg CD, et al. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N Engl J Med. 2011; 365(5):395-409.
- De Koning H, Van Der Aalst C, Ten Haaf K, Oudkerk M. PL02.05 Effects of Volume CT Lung Cancer Screening: Mortality Results of the NELSON Randomised-Controlled Population Based Trial. J Thorac Oncol. 2018;13(10):S185
- Ma J, Ward EM, Smith R, Jemal A. Annual number of lung cancer deaths potentially avertable by screening in the United States. Cancer. 2013;119(7):1381-1385.
- Kinsinger LS, Anderson C, Kim J, et al. Implementation of lung cancer screening in the Veterans Health Administration. JAMA Intern Med. 2017;177(3):399-406.
- Blom EF, Ten Haaf K, Arenberg DA, de Koning HJ. Disparities in receiving guideline-concordant treatment for lung cancer in the United States. Ann Am Thorac Soc. 2020;17(2):186-194.