Treating the whole patient, not just the disease, is a basic tenet of holistic care. Understanding the physical, emotional, and spiritual needs of patients can help providers provide optimal care and improve outcomes. Stress comes in many forms, and some patients need help building resilience and stress-management skills.
A New Approach to Assessing Patients’ Fitness and Disability Levels
Many older patients with lung cancer would prefer to mitigate disability rather than prolong their lives. High daily quality of life sometimes outweighs survival benefit, which is not always the assumption made by healthcare providers. There is a lack of research in this area, which led Carolyn J. Presley, MD MHS, and Nicole A. Arrato, MA, of The Ohio State University Comprehensive Cancer Center to study physical fitness and disability among patients with lung cancer. Ms. Arrato presented the findings during OA08: Putting the Patient at the Center: Holistic Patient Care.
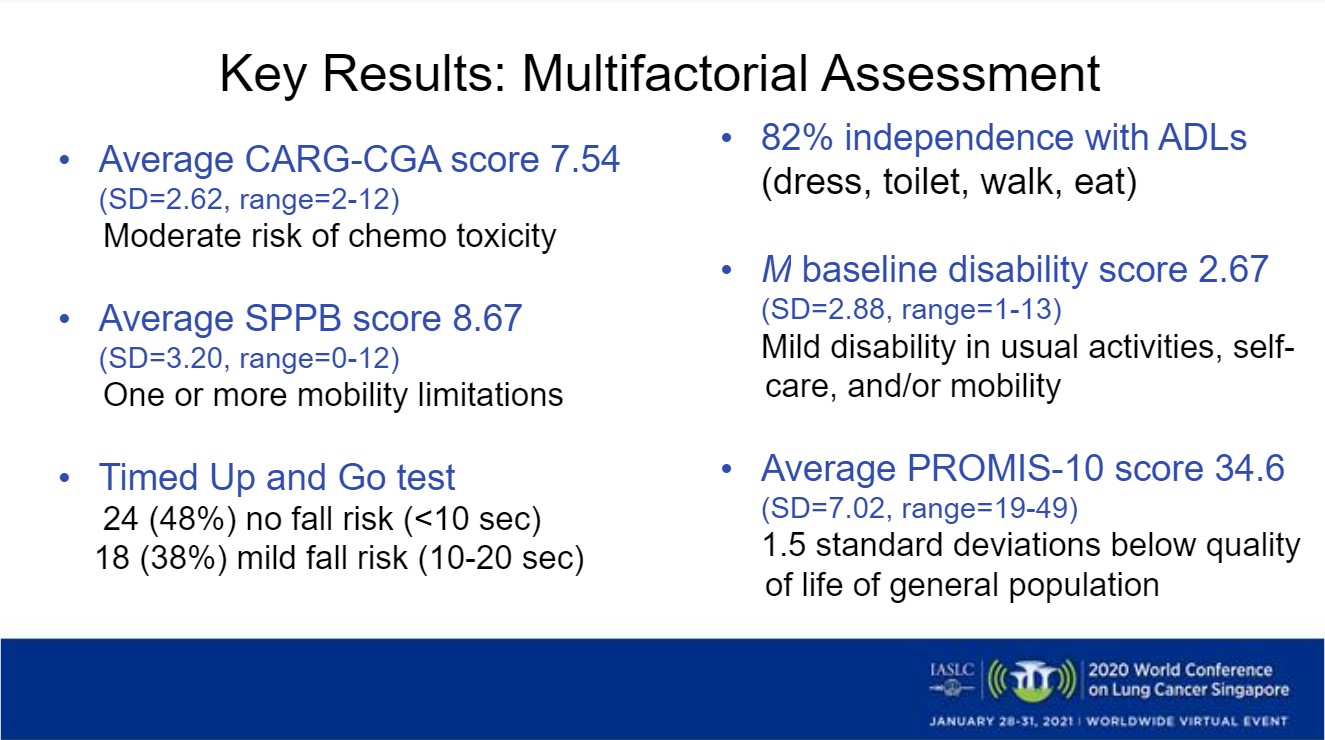
The FITNESS study examined the feasibility of a new approach to assess disability in older adults with lung cancer. They recruited 50 patients with NSCLC who were aged 60 or older and in active treatment. The aim was to conduct a multifactorial assessment using a variety of tools to measure how well patients were able to move around and perform daily tasks for themselves (Figure).
The FITNESS Findings
The study found that out of the 50 patients, mosts demonstrated at least one mobility limitation. When patients were tested from a seated position to standing and walking a short distance across a room, about one-half were at the least risk for falling, and 18 were at a slightly higher risk for falling. Falls can lead to hospital stays, so this is an important piece of data. Of the 50 patients, 82% were able to independently complete basic tasks such as dressing, bathing, and using the toilet.
“The FITNESS study approach could transform the standard of care when it comes to controlling disability and promoting resilience, allowing patients to stay at a level of function where they start [at baseline] and even to get better,” Ms. Arrato said.
Being physically independent can be a shared goal for patients and their medical team.
“This [new approach] allows providers to identify patients who are presently more disabled and maybe even at risk for future disability and falls,” Ms. Arrato said.
Patient-Centered Care
Discussant Andreas Charalambous of Cyprus University of Technology, Cyprus, and the University of Turku, Finland, talked about the importance of patient-centered care, which requires a true partnership between patients and their healthcare providers so that the individual’s needs and aspirations drive healthcare decisions.
“Multimodal and personalized interventions are essential in addressing the complex and diverse needs of patients across the care continuum,” he said.
Patient-centered care includes the following dimensions:
- Respect for patient preferences
- Coordination and integration of care
- Information and education
- Physical comfort
- Emotional support
- Involvement of family and friends
- Continuity and transition
- Access to care
Dr. Charalambous discussed two studies that looked at patients’ psychological as well as physical symptoms during cancer care in relation to overall outcomes. He discussed illness perception profiles—assessments of patients’ beliefs and feelings they have at diagnosis and during treatment. One study showed great variability in outcomes, and Valentine et al. examined how the variances in illness-perception profiles were related to outcomes. Although not conclusive, with further research it could be an important future predictor of outcomes. Dr. Charalambous highlighted the importance of a holistic approach, where it is acknowledged that there is a strong relationship between body, mind and spirit, so as to better understand each patient as an individual and understanding each patient’s psychological well-being would be a keystone.
A second study by Labuc et al. looked at common symptoms such as cancer-related fatigue and how they can affect the physical as well as the cognitive abilities of a patient in active treatment. It is not only the cancer itself, but also the myriad side effects such as fatigue, that can be improved with a multimodal approach. Occupational therapy, for example, can play a role in mitigating fatigue and helping patients feel more energized.
Continued interest in treating the whole patient, at the point of diagnosis and with a multimodal approach, illustrates that standard of care is evolving and quality of life is improving for patients with lung cancer.
This session had a real-time Q&A that provided attendees with the opportunity to ask questions of the session participants. The Q&As are included in the On-Demand recordings, available through the virtual platform. Registration is ongoing for the next 90 days at wclc2020.iaslc.org.