With the approval of taletrectinib in 2025, several frontline TKIs are now available for treating patients with ROS1-altered non-small cell lung cancer (NSCLC). However, given the resistance to frontline TKIs and tolerance issues with currently available therapies, new options are needed in this setting.
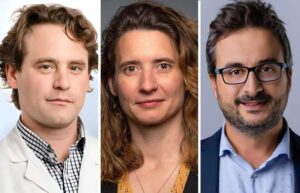
Alexander E. Drilon, MD, lead study author and Chief of the Early Drug Development Service at Memorial Sloan Kettering Cancer Center in New York, explained the rationale for the evaluation of zidesamtinib in ARROS-1 during the first of two Presidential Symposia at the 2025 World Conference on Lung Cancer (WCLC).

Presidential Symposium 1 with Lectureship Award Presentations
It’s not too late! With on-demand access, registered WCLC 2025 attendees can still watch Alexander E. Drilon, MD, and others present much-awaited data during the first of two Presidential Symposia. LEARN MORE
“Zidesamtinib is a highly ROS1-selective TKI designed to surpass the limitations of prior ROS1 TKIs,” Dr. Drilon said. “The drug is highly potent against ROS1 and ROS1 TKI-resistant mutations, has optimal CNS coverage, and avoids tropomyosin receptor kinase (TRK) inhibition.”
He said highly ROS1-selective TRK-sparing TKIs can help avoid adverse neurologic effects of TRK inhibition.
Dr. Drilon shared findings from pivotal analyses in the phase 1/2 global, single-arm ARROS-1 trial of zidesamtinib in ROS1-altered advanced NSCLC.He discussed the safety population, which comprised 432 patients who had received the recommended phase II dose of zidesamtinib (100 mg once daily), and the efficacy population, which included 117 patients who had received prior ROS1 TKI therapy. Dr. Drilon also shared the first disclosure of efficacy for TKI-naïve patients.
Dr. Drilon said, “Of note, almost half (49%) of the [ROS1 TKI-pretreated] patients had active CNS disease and more than a third (36%) had a secondary ROS1 mutation, including G2032R.” Additionally, half had received one prior TKI, primarily crizotinib or entrectinib, while the other half had received ≥ 2 prior TKIs, including lorlatinib, repotrectinib, and taletrectinib.
The primary endpoint, overall response rate (ORR), was 44% in TKI-pretreated patients, with a 12-month duration of response (DOR) rate of 78%. The ORR was 55% in the 55 patients who had received only one prior TKI, with a 12-month DOR rate of 93%.
“The ORR in patients who had received ≥ 2 prior TKIs was 38%. And acknowledging the smaller denominator for pretreatment with the more recently approved drugs repotrectinib and taletrectinib, it is highly encouraging to see durable responses in these patients for whom no targeted therapy is currently approved,” Dr. Drilon said.
Zidesamtinib was also active against “historically recalcitrant G2032R resistance mutation,” with an ORR of 54% and 83% in patients who received up to four or only one prior ROS1 TKI, with or without chemotherapy.
In patients with measurable CNS lesions at baseline, the intracranial response was 85% in patients who received one prior ROS1 TKI, with or without chemotherapy. Notably, zidesamtinib also yielded intracranial responses in 48% of patients who had received up to four prior ROS1 TKIs, including other brain-penetrant TKIs.
Dr. Drilon also shared the first disclosure of preliminary efficacy findings for 35 TKI-naïve patients with an ORR of 89%, including three complete responses. These results support continued investigation of zidesamtinib in the frontline setting, he noted.
The safety analyses showed that zidesamtinib was generally well tolerated, with low rates of dose reductions (10%) and discontinuation (2%). The most common treatment-emergent adverse events included peripheral edema, constipation, creatine phosphokinase increase, fatigue, and dyspnea, with a low overall frequency of grade ≥ 3 events.
Anne-Marie C. Dingemans, MD, PhD, Professor of Thoracic Oncology at Erasmus Medical Center Rotterdam, Netherlands, who interpreted the results, reviewed the current landscape of ROS1 TKIs and compared key features of approved TKIs active in ROS1-altered NSCLC with those of zidesamtinib.
Although the responses with zidesamtinib in patients exposed to up to four prior TKIs are lower than that for patients treated with one prior TKI, primarily crizotinib, the DOR was “impressive,” Dr. Dingemans said, “with the majority, nearly all patients, having responses for more than 18 months, which seems more durable than with repotrectinib and taletrectinib.”
These data are important, despite the limited numbers, given the changing frontline ROS1 TKI landscape, she added.
Contextualizing the CNS responses, Dr. Dingemans said it is important to have a drug that is active in the setting of brain metastases, as up to a third of patients with ROS1-altered NSCLC have CNS lesions at diagnosis, and most crizotinib failures in such patients occur in the brain.