It is well known that ongoing tobacco use is associated with poorer survival in patients with cancer, and the IASLC has emphasized this message.1 The Declaration from IASLC: Tobacco Cessation After Cancer Diagnosis reminds us that tobacco assessment and cessation support are key components of cancer care. Over the past months, COVID-19 has swept the globe, with cases still rising in many countries. Unfortunately, there is no vaccine for prevention and no standard proven pharmacologic treatment other than supportive care. Non-pharmacologic interventions include school and other business closure, frequent hand hygiene, wearing masks in public, and encouraging people to remain home. As the pandemic has progressed, we have learned about risk factors for poorer outcomes. Those with advanced age, chronic lung or heart disease, diabetes, or obesity are at increased risk of complications and death from COVID-19. Chemotherapy, immunosuppressant medications, or immunologic diseases could potentially lead to increased risk from infection. Our patients with cancer—particularly those with lung cancer—may be a particularly vulnerable group. Advanced age, medical comorbidities (particularly respiratory disease), and altered immune function may be a perfect storm of risk. Although most factors cannot be altered, there is one particular alterable risk that may often be overlooked by patients and physicians: smoking or vaping.
Smoking and COVID-19
COVID-19 is often spread via droplets, and advanced cases lead to respiratory failure. For those who smoke, frequent hand-to-mouth contact and increased coughing could be additional factors for transmission. Low levels of smoking or even secondhand smoke have previously been linked to poorer outcomes in acute respiratory distress syndrome.2,3 Smoking results in poorer outcomes in those with bacterial pneumonia or influenza; now we are learning that smoking can pose significant risks in those with COVID-19. A meta-analysis of 9,025 patients with COVID-19 demonstrated that smoking was associated with poorer outcomes (OR 2.25, 95% CI [1.49, 3.39]; p=0.001).4 Mucociliary clearance is an important barrier to respiratory infections. Smoking creates thicker mucus and paralyzes the cilia, preventing transport of mucus out of the lungs. This is associated with worsening infections, but these changes are reversible with cessation.
E-Cigarettes
Electronic cigarettes have gained popularity in many countries through a perception of less health risk. Although e-cigarettes may contain less carcinogens than cigarette smoke, they are associated with health risks, particularly in terms of respiratory infections.5 E-cigarettes can suppress immune function, impair mucus clearance, and weaken response to infection.5,6 We do not have clear long-term data about e-cigarette use, but evidence-based cessation strategies should be used to help patients quit smoking, and patients who are vaping should be encouraged to quit.
Importance of Cessation
At this point, we have to remember the criticality of addressing tobacco in cancer care and also realize that patients may be more vulnerable than ever to respiratory infections. Benefits of cessation may be crucial for our population at this time. There are numerous benefits from quitting smoking including decreased risk of cancer or heart attack; however, improved respiratory function is one of the benefits seen soonest after quitting.7 It is our role as clinicians to ask every patient about use on each visit and to guide them toward evidence-based care. If we do not ask, patients may falsely assume it is not important.
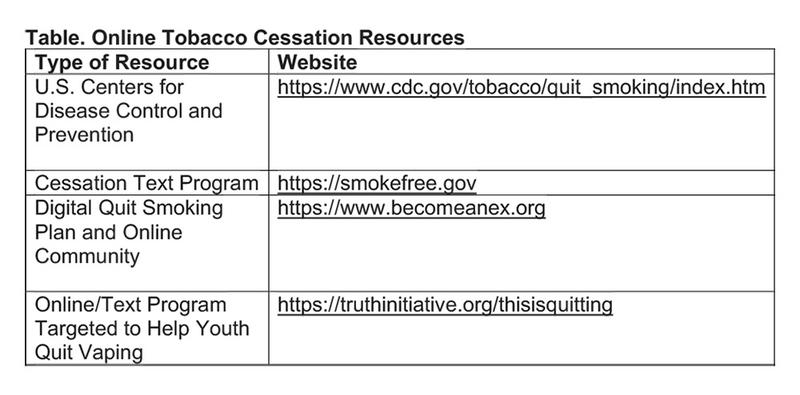
Some patients quit unaided or “cold turkey” by stopping abruptly. If this can work, it may be the simplest method of cessation, but many patients do not remain abstinent without support. During this time, some aspects of the pandemic may be barriers to cessation, whereas some aspects may actually support cessation. Remaining at home means no interaction in bars and other places where people may smoke. Essential businesses include grocery stores and pharmacies. Financial challenges may provide more incentive to kick a costly habit. However, boredom, anxiety, or stress associated with health and economic challenges may increase cravings. Fortunately, many resources are free of charge either online or by telephone and are accessible without leaving the home. Nearly every country has a telephone quitline providing free guidance by trained experts. Many other resources exist online, and a few are listed in the Table.
Each medical practice is unique in terms of resources available in that community, and physicians need to take an active role to assure that they are using the best available resources to help patients.
Pharmacotherapy Support
In addition to telephone counseling or support from another program, many who smoke benefit from medication to support a quit attempt. The most common types of pharmacotherapy are nicotine-replacement therapy (NRT). Patches are the most commonly used NRT. They are slow acting, providing steady administration for several hours. Gum or lozenge forms of NRT provide a faster delivery of nicotine, which can help when cravings hit. Patches, gum, and lozenges are available over the counter in pharmacies and some grocery stores. Details regarding side effects are available online or can be discussed with a pharmacist or cessation expert through the quitline, but in general, NRT is certainly safer than smoking. Some strategies include “combination NRT” with a patch as a baseline dose, supplemented with gum or lozenge for breakthrough cravings. It is important to note that although e-cigarettes do contain nicotine, they are not an approved NRT. Medications such as varenicline (Chantix® and Champix®) or bupropion (Zyban® and Wellbutrin®) are available by prescription and also improve cessation success .
Lasting Effects
At this point, we are seeing the significant effects of COVID-19 on our health care systems and certainly need to mitigate risk systemically in any ways possible. Decreasing incidence of COVID-19 infections though distancing and less contact is crucial. Smoking cessation may play a role in reducing the risk of infection and decreasing severity for those who do get it. For those who quit and improve lung function, this could make a difference between recovering at home versus needing hospitalization; it may make a difference for someone who is hospitalized and stabilizes versus someone who progresses to needing intensive care. We are constantly learning about best practices of treating this viral pandemic. This pandemic is sharply rising in many places, but we do forecast a time when it will decrease and risks of COVID-19 will drop. However, the benefits of cessation will not end when this pandemic passes. In addition to hand washing, distancing, and staying at home, quitting now is one of the healthiest steps people can take, and this will have continued benefits for years to come. For our patients who may have particular vulnerability to this respiratory viral pandemic, this is a crucial time. Fortunately, many of the tools to aid cessation are conveniently available, even when staying at home. It is our role to use every means possible to improve outcomes in our patient population.
References:
1. International Association for the Study of Lung Cancer. Declaration from IASLC: Tobacco Cessation After Cancer Diagnosis. Published September 4, 2019. Accessed April 27, 2020. https://www.iaslc.org/About-IASLC/News-Detail/declaration-from-iaslc-tobacco-cessation-after-cancer-diagnosis.
2. Calfee CS, Matthay MA, Kangelaris KN, et al. Cigarette smoke exposure and the acute respiratory distress syndrome. Crit Care Med. 2015;43(9):1790.
3. Hsieh SJ, Zhuo H, Benowitz NL, et al. Prevalence and impact of active and passive cigarette smoking in acute respiratory distress syndrome. Crit Care Med. 2014;42(9):2058.
4. Patanavanich R, Glantz SA. Smoking is Associated with COVID-19 Progression: A Meta-Analysis. medRxiv Published April 6, 2020. Accessed April 27, 2020. https://www.medrxiv.org/content/10.1101/2020.04.13.20063669v1.full.pdf+html.
5. Gotts JE, Jordt SE, McConnell R, Tarran R. What are the respiratory effects of e-cigarettes? BMJ. 2019;366:l5275.
6. Martin EM, Clapp PW, Rebuli ME, et al. E-cigarette use results in suppression of immune and inflammatory-response genes in nasal epithelial cells similar to cigarette smoke. Am J Physiol Lung Cell Mol Physiol. 2016;311(1):L135-44.
7. Centers for Disease Control and Prevention. Benefits of Quitting. Updated December 11, 2017. Accessed April 27, 2020. https://www.cdc.gov/tobacco/quit_smoking/how_to_quit/benefits.
The Campaign for Tobacco-Free Kids is an organization working to reduce global deaths from smoking and smoking rates. For more than 20 years, the organization has worked at national, state, and local levels within the United States, as well as internationally in low- and middle-income countries at highest risk from tobacco use to provide advocacy and public health policy changes.
Although tobacco still kills nearly 8 million people worldwide, the Campaign for Tobacco-Free Kids boasts a robust portfolio of international initiatives, ranging in focus from taxation and pricing to smuggling. Specific to the United States, resources for parents about e-cigarettes and vaping are available for download.
The Global Legal Center provides expert technical assistance and resources to tobacco control lawyers and advocates working to help countries pass and implement evidence-based policies based on the WHO Framework Convention on Tobacco Control. The Campaign’s team of lawyers, known as the International Legal Consortium, provides assistance in drafting and defending tobacco control laws and works to build the capacity for tobacco control efforts in low- and middle-income countries.
To get involved in international efforts, visit tobaccofreekids.org.
IASLC’s Official Podcast Program, Lung Cancer Considered, on Tobacco Control
Tune in each month to hear conversations among researchers, health care professionals, patients, and advocates who are making a different in the care of patients with thoracic cancers. New episodes are released the first and third Monday of each month and are available for download at https://soundcloud.com/lungcancerconsidered.
- Moderator Dr. Jack West and guest Dr. Rafael Meza discuss the recent Journal of Thoracic Oncology study, “Potential Impact of Cessation Interventions at the Point of Lung Cancer Screening on Lung Cancer and Overall Mortality in the United States.” Dr. Meza is an associate professor in the department of epidemiology and co-leader of the cancer epidemiology and prevention program at the University of Michigan Rogel Cancer Center.
- IASLC CEO David Mesko and Dr. Matt Steliga, chair of The IASLC Tobacco Control and Smoking Cessation Committee and a surgical oncologist at Winthrop P. Rockefeller Cancer Institute, discuss IASLC’s leadership regarding e-cigarettes and vaping.





