The IASLC 2025 Hot Topic in Basic & Translational Science Small Cell Lung Cancer (SCLC) meeting recently convened in New York City, marking a decade since the conference first began. Charles Rudin, MD, PhD, Deputy Director at the Memorial Sloan Kettering Cancer Center, took the stage to deliver the keynote address.

Registered attendees can access the on-demand recording and other meeting coverage on the IASLC’s Lung Cancer 360.
He opened by assessing the current state of SCLC, citing positive trends that have been revealed by the Surveillance, Epidemiology, and End Results (SEER) registry, which indicate a decline in SCLC incidence in the United States.
“We’re making tremendous progress in terms of reducing small cell incidence in the United States. And this, of course, really reflects tobacco use in this country,” Dr. Rudin said.
He noted that these encouraging trends haven’t been observed globally yet; however, that may be due to a lack of data.
Dr. Rudin pivoted to challenges in limited-stage SCLC, such as appropriate criteria for surgery.
“We need to define what the appropriate indications for surgery are now in the modern age of better imaging, where we’re not including a lot of patients with extensive-stage disease in what we’re calling limited stage,” Dr. Rudin said.
Other important questions included the declining use of prophylactic cranial radiation in practice, its relevance in the stereotactic radiation era, and the role of newer drugs in patients with metastatic disease.
Dr. Rudin stressed the impact of immunotherapy on survival and how far research has come in extensive-stage SCLC.
“If we look back at the prior era where we didn’t have immunotherapy, these [survival] curves really went to ground,” he said. “Today, most patients with metastatic lung cancer still die of disease, but there’s a real tail in these curves, and there’s a tripling of the 3-year survival. I think, most importantly, that tail becomes pretty flat.”
Even so, he said only 10% to 15% of patients with SCLC appear to be immunologically responsive, while the other 85% to 90% don’t appear to benefit.
“We need to sort out those differences. When it works, it can really work,” he said.
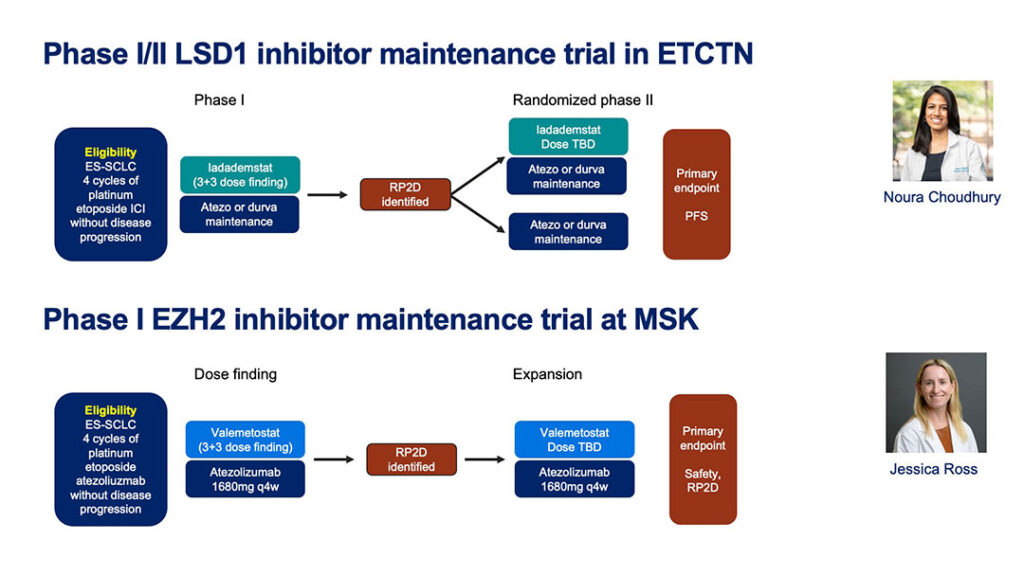
Dr. Rudin also explored two trials underway looking at possible stimulants for immunotherapy: one is exploring LSD1 as a gene-determinant of outcome, the other is an EZH2 approach.
“Both of these trials are small, and they’re going to be signal finding for this event,” Dr. Rudin said. “I think a key part of these will be blood collection prior to treatment and on treatment serially.”
Dr. Rubin also highlighted promising new agents for recurrent metastatic SCLC, including multiple, highly active T-cell engagers and antibody drug conjugates.
“It’s actually a super exciting time,” he said. “I think a key question is, which of these, and in which context, will improve our first-line therapies?”
He closed by highlighting how transcriptionally defined cell states in SCLC are providing novel insights into researchers’ understanding of tumor biology. “Many of the exciting new agents fortunately have activity across the subsets and don’t seem to be subtype-selective,” Dr. Rudin said. He proposed that constraining subtype plasticity could provide some unsuspected therapeutic opportunities, such as with SMARCA4, which is highly expressed in high neuroendocrine SCLC.
“Maybe locking tumors into one subtype gives us an opportunity to more effectively treat the disease,” he said.