According to data presented during the 2023 World Conference on Lung Cancer, intensity-modulated radiation therapy (IMRT) should become the standard approach in combination with chemotherapy for locally advanced non-small cell lung cancer (NSCLC). Five-year follow-up data from the NRG Oncology RTOG 0617 trial showed improved overall survival using IMRT, a 2-fold reduced risk of several pulmonary toxicity, and reduced cardiac toxicity compared to 3-dimensional conformal radiation therapy (3D-CRT)
“We turned the page on 3D-CRT 30 years ago in prostate cancer, head and neck cancer, and brain tumors in favor of IMRT,” said Stephen Chun, MD, Associate Professor of Radiation Oncology at the University of Texas MD Anderson Cancer Center, Houston. “The time has come to turn the page on 3D-CRT for locally advanced non-small lung cancer in favor of IMRT, which delivers clinically meaningful benefits to patients.”
Dr. Chun presented a secondary analysis of RTOG 0617 with 5-year follow-up data during an oral abstract session titled “Next Steps in Locally Advanced NSCLC: Optimizing Techniques & Choosing Populations that Benefit.” The session is available on demand for registered WCLC 2023 attendees through December 31.
Definitive concurrent chemoradiation has long been the standard of care for locally advanced NSCLC, but there has been little agreement as to the most effective approach to radiation therapy. The initial results of RTOG 0617 showed lower rates of pneumonitis with IMRT, Dr. Chun said, but IMRT is more labor intensive and more costly than 3D-CRT. And there are little long-term data directly comparing the two approaches.
RTOB 0671 randomized 482 patients to either 60Gy plus chemotherapy or 74Gy plus chemotherapy with the choice of IMRT or 3D-CRT determined by the treating clinician. Patients were followed for a median of 5.2 years. The primary endpoints were 5-year overall survival (OS), progression free survival (PFS), local treatment failure, and distant metastasis-free survival (DMFS).
Patients in the IMRT arm had more advanced disease, higher pretreatment lung volume to lung ratio, less favorable cardiac location, higher median pretreatment lung volume, and lower heart V40Gy compared to the 3D-CRT group. The median pretreatment lung volume in the IMRT arm was 59 mL larger than in the 3D-CRT arm, the equivalent of a double centrifuge tube.
“The deck was stacked against IMRT,” Dr. Chun said. “However, we still saw improved overall survival with IMRT, improved PFS, and improved DMFS compared to 3D-CRT. And there was no evidence of excess second malignancies in the IMRT group.”
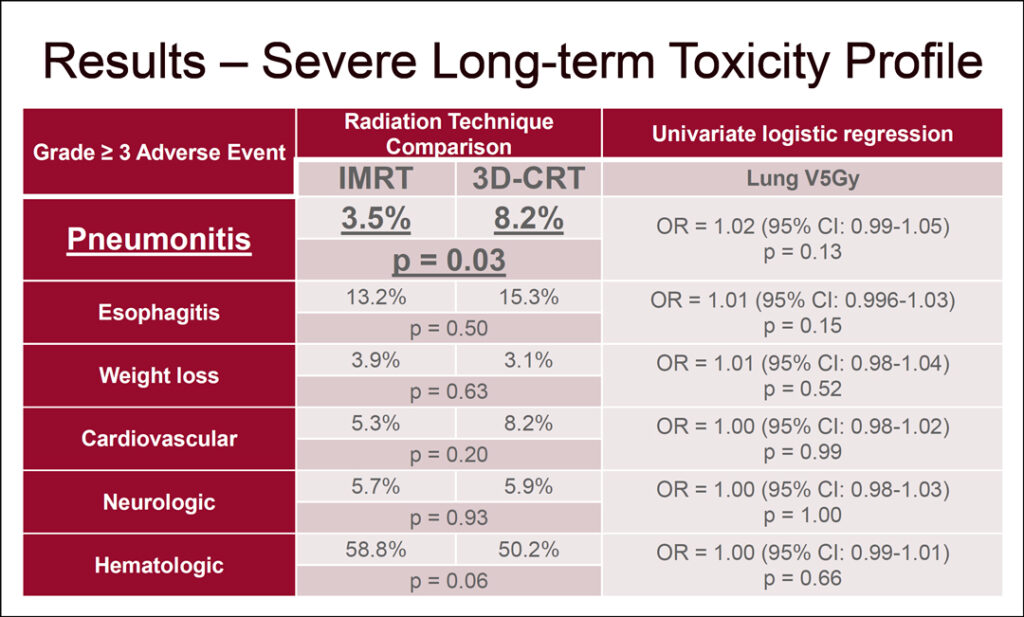
IMRT was associated with more than a 2-fold reduction in severe pneumonitis, 3.5% for IMRT versus 8.2% for 3D-CRT (p=0.03). There was no evidence of any severe toxicity outcomes associated with a low dose lung bath, lung V5Gy. (See Fig. 1)
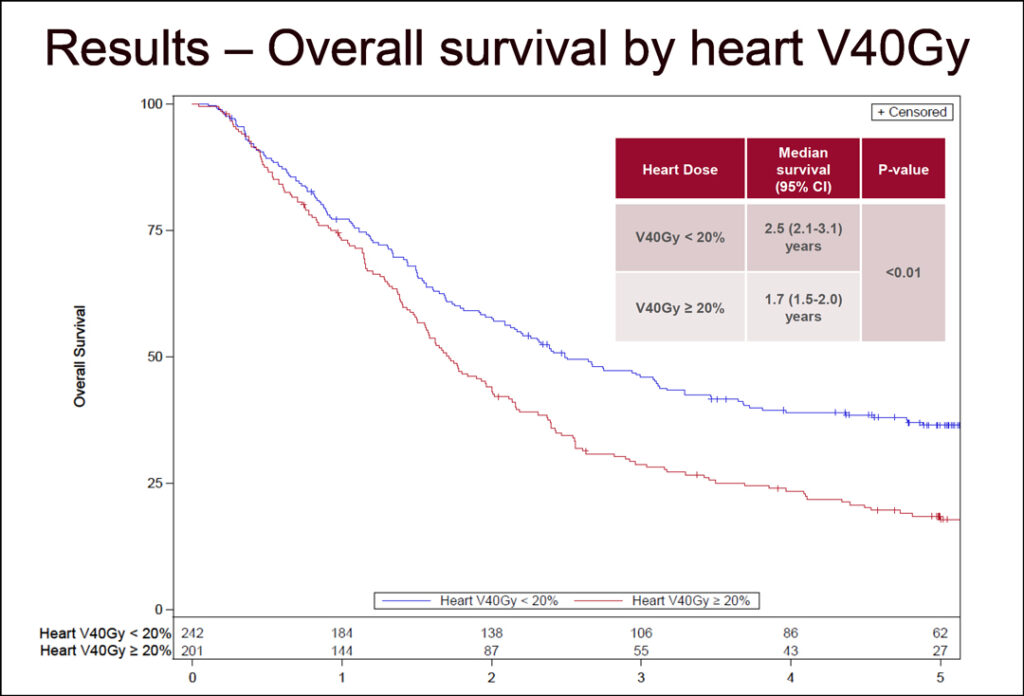
Heart doses of V20Gy, V40Gy, and V60Gy were continuously associated with improved overall survival. Dr. Chun said a heart dose of V40Gy <20% emerged as a novel cardiac restraint and was associated with median OS of 2.5 years versus 1.7 years for a heart dose of V40Gy >20% (HR=1.34, p=0.01). The survival curves began to diverge about 2 years after treatment, he said. (See Fig. 2)
A lower radiation dose of 60Gy was associated with improved survival compared to 74Gy, HR=1.28 (p=0.03). There was no survival difference based on pretreatment lung volume, lung V5Gy, or age.
“This likely represents the strongest evidence we will ever have given that a randomized, controlled trial comparing the two techniques directly is unlikely ever to be performed,” Dr. Chun said. “Age should not be a contraindication or used as a factor to discriminate against patients in the use of chemoradiation for locally advanced NSCLC.”