In his keynote address during the IASLC 2020 Hot Topic Meeting: Liquid Biopsy, co-chair Christian Rolfo, MD, PhD, MBA, provided an overview of the fastpaced evolution of liquid biopsy. In 2018, at the time of initial discussions, it was only used for treatment-naive patients for whom tissue biopsy was insufficient or after acquired resistance to first- or second-generation EGFR TKIs. Since then groundbreaking research articles in the field have been published including the NILE study, which first mentioned the idea of “blood first” and validated cell-free (cf)DNA as equivalent to tissue biopsy, with a more rapid turnaround time for genotyping.1 This was followed closely by reports on new technologies2 and techniques,3 which illustrated further clinical confidence and applications for this procedure. Most recently, two next-generation sequencing (NGS) companion diagnostics have also been approved, providing the ultimate validation of the method.
Dr. Rolfo discussed the importance of liquid biopsy as real time monitoring tool. As observed in the subanalysis of the FLAURA trial,4 showing that circulating-tumor (ct)DNA clearance is associated with improved outcomes in EGFR-mutated NSCLC treated with osimertinib, a recent study demonstrated the utility of ctDNA to predict the outcome of patients who had received long-term PD-(L)1 blockade (> 12 months).5 In this study, tumor tissue was available for 24 patients and was collected for wholeexome (n = 18) or targeted sequencing (n = 6). Blood samples were collected at a median of 26.7 months after initiation of therapy for a total of 31 patients with long-term benefit from PD-(L)1 blockade. Of the 27 patients with undetectable ctDNA, 25 have remained progression-free while all four patients with detectable ctDNA eventually experienced disease progression (Fisher P < 0.0001; 95% CI: 0.51-1). This study provides the rational for tailored treatment strategies in long-term responders to immunotherapy, favoring treatment discontinuation in patients with undetectable ctDNA levels and consolidative treatments in case of ctDNA persistence.
The role of liquid biopsy is rapidly growing in gene-fusion positive NSCLCs, as recently observed in the BFAST trial, which incorporated liquid biopsy into its elegant design. This is one of the first prospective trials using cfDNA for patient selection. More than 2,000 patients with untreated NSCLC were tested, and approximately 1 in 20 were found to have ALK rearrangements using this method and most of them received oral alectinib. Further, more than 75% of these patients were progression-free 1 year later.6
This concept has been extended into real-time monitoring of patients for treatment resistance, and this method is already included in new data for this trial.
New Additions to Consensus Statement
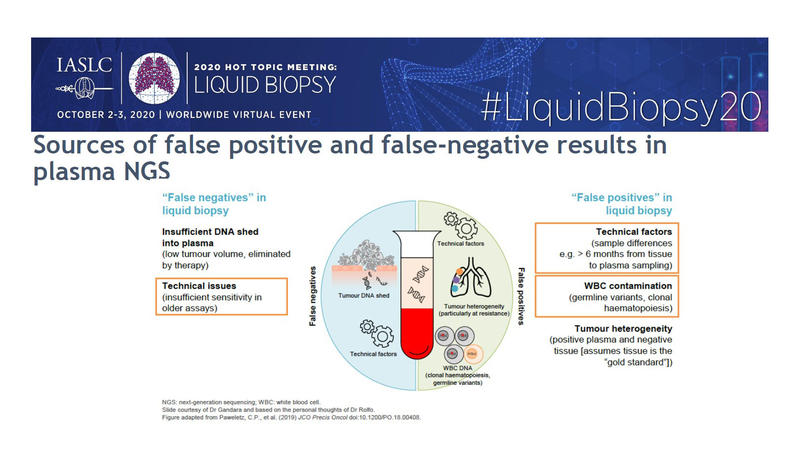
The IASLC Consensus Statement on liquid biopsy, which is expected to be completed by the end of the year, will include information about KRAS as a prognostic and predictive biomarker, hopefully elucidating which patients will benefit from therapy with sotorasib. Complicating factors involving KRAS, such as clonal hematopoiesis, will be discussed and the statement will provide clarity regarding the possible false positive/negative results from plasma NGS.
Statement authors, including Dr. Rolfo, will also include a section for research and future perspectives. The IASLC will offer a webinar discussing liquid biopsy in early lung cancer detection, as well as illustrating how liquid biopsy can be used in the detection of minimal residual disease, and what new techniques, such as use of exosomes, ctRNA, and platelet-derived nucleic acids, also play an important role as biomarkers and in the understanding of lung cancer. Other topics that the statement hopes to cover include the role of liquid biopsy in determining T-cell receptors and major histocompatibility complex class I and II specific sequences in the context of immunotherapies (potentially including vaccines), its increased and improved use in clinical trials, and its use in SCLC, where tissue biopsies have been prove challenging.
References:
1. Leighl NB, Page RD, Raymond VM, et al. Clinical Utility of Comprehensive Cell-free DNA Analysis to Identify Genomic Biomarkers in Patients with Newly Diagnosed Metastatic Non-small Cell Lung Cancer. Clin Cancer Res. 2019;25(15):4691-4700.
2. Pritchett MA, Camidge DR, Patel M, et al. Prospective Clinical Validation of the InVisionFirst-Lung Circulating Tumor DNA Assay for Molecular Profiling of Patients With Advanced Nonsquamous Non-Small-Cell Lung Cancer. JCO Precision Oncol. Epub 2019 April 25. DOI: 10.1200/PO.18.00299.
3. Schrock AB, Welsh A, Chung JH, et al. Hybrid Capture-Based Genomic Profiling of Circulating Tumor DNA from Patients with Advanced Non-Small Cell Lung Cancer. J Thorac Oncol. 2019;14(2):255-264.
4. Zhou C, Imamura F, Cheng Y, et al. Early clearance of plasma EGFR mutations as a predictor of response to osimertinib and comparator EGFRTKIs in the FLAURA trial. J Clin Oncol. 2019 May 20;37(15_suppl):9020–9020.
5. Hellmann MD, Nabet BY, Rizvi H, et al. Circulating tumor DNA Analysis to Assess Risk of Progression after Long-term Response to PD-(L)1 Blockade in NSCLC. Clin Cancer Res. 2020;26(12):2849-2858.
6. Gadgeel SM, Mok TSK, Peters S, et al. Phase II/III blood first assay screening trial (BFAST) in patients (pts) with treatment-naive NSCLC: initial results from ALK+ cohort. Ann Oncol. 2019;30(suppl 5): LBA81_PR.






