Even the most advanced CT scanners available face limitations in their ability to measure small lung nodules. This is a concern since small errors in two-dimensional measures can quickly balloon to become large errors in predicted volume change.
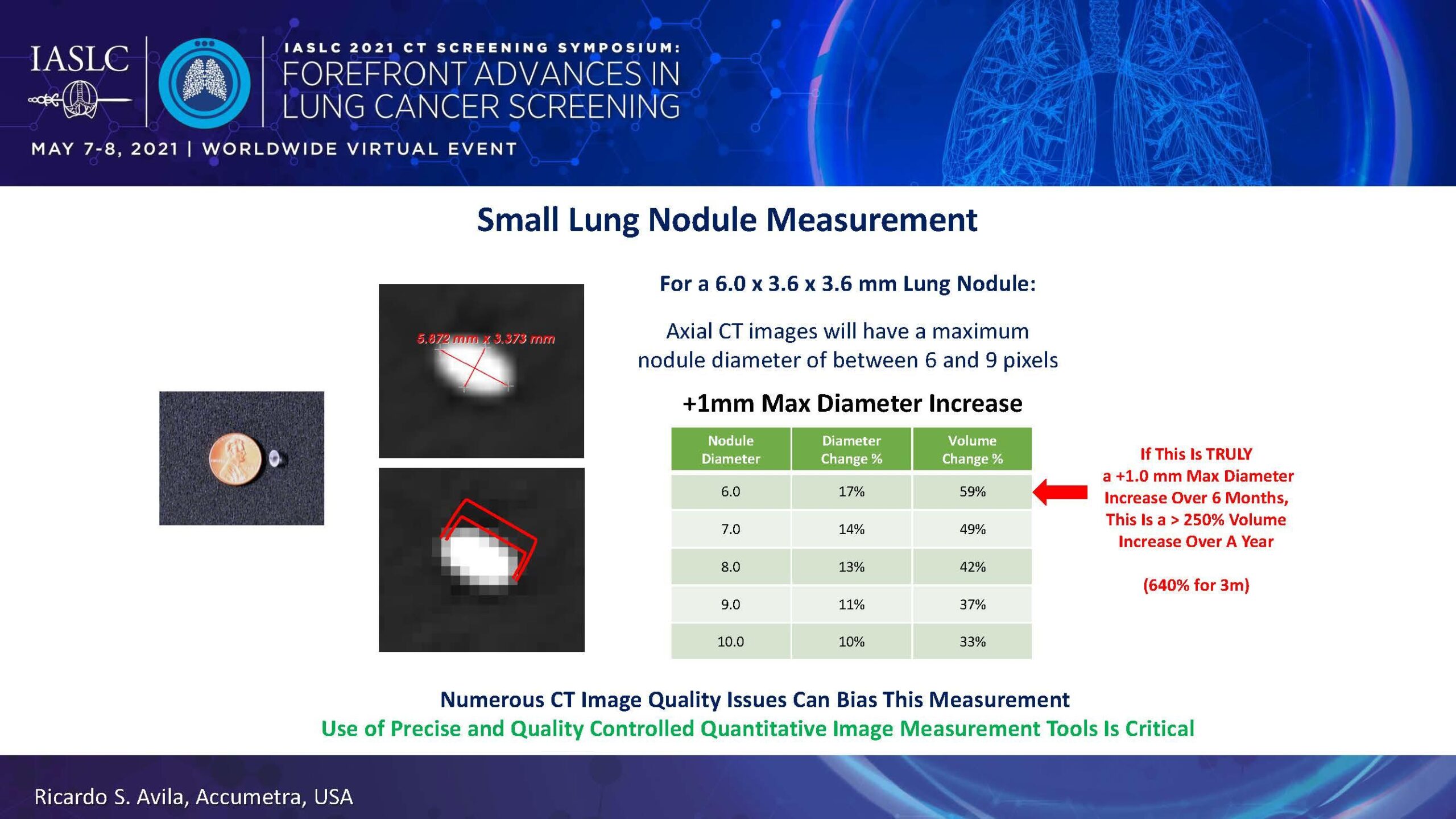
As Ricardo S. Avila, of Accumetra, LLC, explained, an axial CT image of a 6.0 by 3.6 by 3.6 mm lung nodule will have a maximum nodule diameter ranging between 6 and 9 pixels. If the resolution is off by roughly half a pixel on each side, this results in about a 1-mm increase, translating to a 59% increase in volume.
“Unless you quality-control the imaging and even the software, it will be difficult to determine the rapidly growing lung cancers or nodules from those that are benign,” Mr. Avila said.
CT Image Quality Issues
Mr. Avila noted that currently available CT scanners are dogged by numerous quality-related issues that can greatly affect small (6-10 mm) lung nodule measurements. These include degraded image quality in the periphery, spatial warping along the Z dimension, Hounsfield Unit values that vary depending on the reconstruction kernel used, discrepancies in slice thickness when requesting thin slices (≤1 mm), and loss of resolution with lowered radiation doses.
Mr. Avila also stressed that CT imaging technology is constantly changing in terms of scanner geometries and detectors, “standard” reconstruction kernels, iterative reconstruction algorithms, and so forth. “So it’s really important that clinical sites have tools to understand when their systems are stable and reproducible and when they’re not,” he emphasized.
Mr. Avila shared research he helped conduct during the phase 2 ABIGAIL trial of first-line bevacizumab plus chemotherapy in nonsquamous non-small-cell lung cancer. The group placed “pocket phantoms”—1.6-cm Teflon spheres—on the chest of patients being scanned to determine the accuracy of the CT machines being used. They found that some scanner models returned warped images of the spheres that resulted in up to a 44% change in nodule volume (Fig. 1).1
“This was a real eye-opener, and it forced us to look more carefully at what’s going on in CT scanners,” Mr. Avila said. He also noted that although this study was conducted in 2010, these same scanners are still used today for lung cancer screening, suggesting this is a persisting problem.
QIBA Efforts to Improve CT Image Quality
To overcome problems like this, the Quantitative Imaging Biomarkers Alliance (QIBA), under the auspices of the Radiological Society of North America (RSNA), has endeavored to increase the accuracy and reproducibility of quantitative imaging by minimizing variability across devices, sites, and patients. As part of these efforts, QIBA created a profile of fundamental CT image properties that all sites should aim to implement when assessing lung nodule volume with low-dose CT screening (Fig. 2).
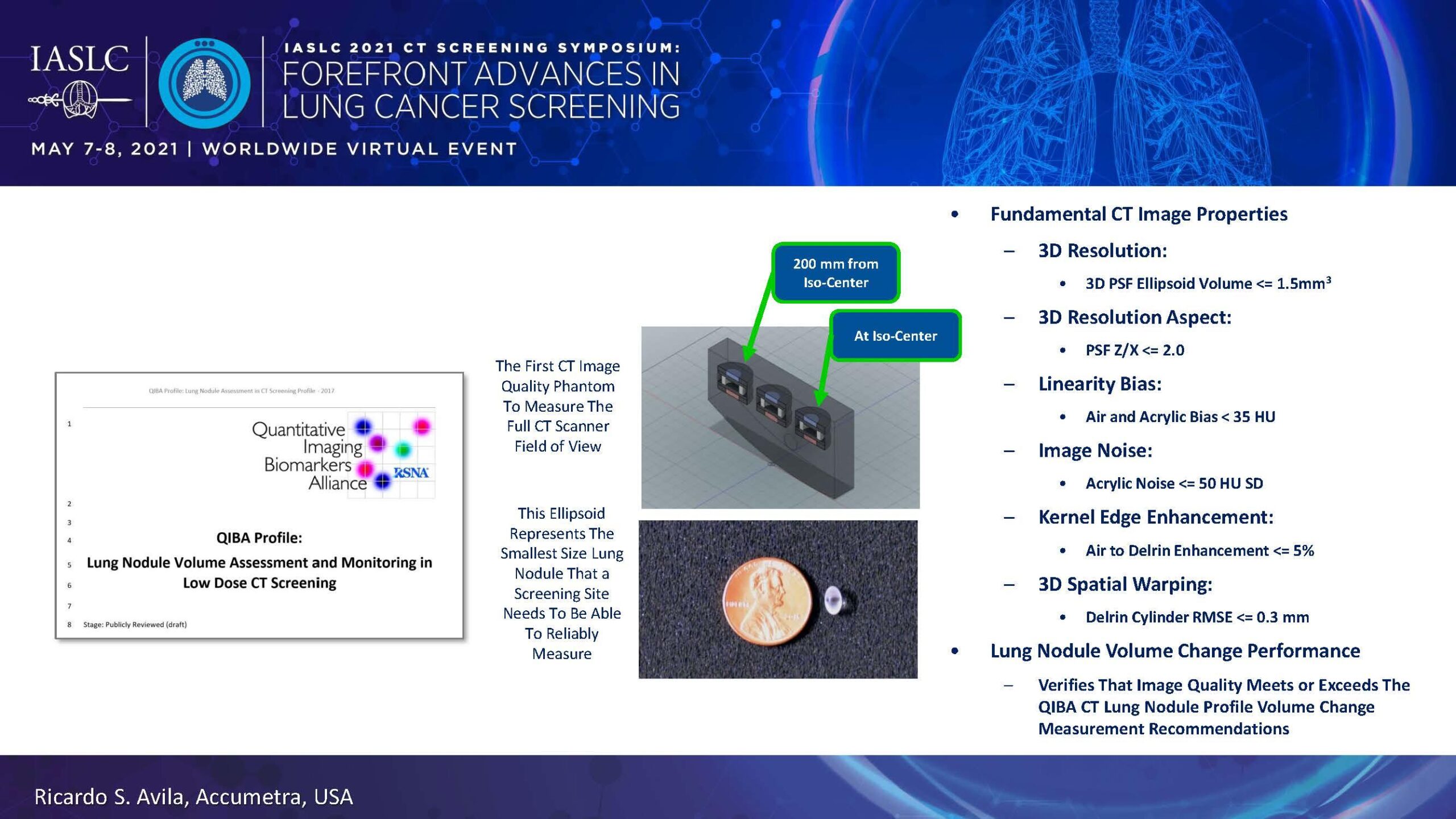
In addition, QIBA helps sites check the accuracy of their scanners and troubleshoot, if necessary. The process is simple: Sites scan a low cost calibration phantom provided by QIBA using their current protocol for measuring lung nodules. The information is sent to QIBA, and within a few minutes an automated report is returned detailing the quality of the CT scan.
“If they run into a problem, we consult with them and help them optimize the protocol so that they get better results and then test it again until they’re passing,” Mr. Avila said.
Those sites that meet all requirements receive conformance certification from QIBA/RSNA documenting their ability to achieve high-quality quantitative imaging results. QIBA also encourages regular reassessments so that sites can maintain records of how their scanners perform over time to ensure quality control.
QIBA continues to devise new strategies to better support high-quality imaging. For example, the group has created a new phantom device that consists of thick wall of water surrounding a core that can house small manufactured nodules. Mr. Avila says that using this device, which weighs 9 kg (20 lbs) when filled with water, can provide sites with guidance on the quality of small lung nodule images when scanning a large patient, especially when trying to lower the radiation dose.
QIBA is also generating a tool that determines the minimum time to wait between scans for a given patient based on the size of the nodule and the accuracy of the CT scanner. The aim here is to lower follow up times while maintaining confidence that a nodule that appears to be rapidly growing is indeed doing so and is not an imaging artifact.
According to Mr. Avila, the bottom line is that QIBA’s tumor phantoms and services “allow sites to eliminate the low-quality CT scans that are pretty common throughout the world.”
- 1. Henschke CI, Yankelevitz DF, Yip R, et al. Tumor volume measurement error using computed tomography imaging in a phase II clinical trial in lung cancer. J Med Imaging (Bellingham). 2016;3(3):035505.






