The social and emotional needs of patients are increasingly being recognized as equally important to their physical needs, and use of multidisciplinary teams is helping to bridge the gaps between clinical and psychosocial care. The Education Session “Practice Changing Initiatives” (ES11) addressed exciting initiatives to move the field forward while helping patients become better advocates for themselves.
Psychological Needs
Presenter Lisa Burgess, PhD, a psychologist at the Phoenix VA Health Care System discussed ways to encourage people to better understand their risks for lung cancer and to get screened periodically. She emphasized the importance of multidisciplinary teams in helping patients with the emotional toll of screening and diagnosis.
“We want to encourage patients to know where they are in their risk stratification, … use that as a gateway to engage in screening, … and stay with that process to get re-screened at intervals that are recommended for them,” Dr. Burgess said.
It is important to understand diverse patient populations, Dr. Burgess said, such as being aware that people with mental illness use tobacco products at a higher rate than others and have a higher morbidity rate.
The stigma associated with use of tobacco products has been and remains a barrier for patient-initiated screening. Despite the fact that the United States Preventive Services Task Force guidelines now recommend that people with at least a 20 pack-year smoking history who are aged 50-80 and who quit smoking in the past 15 years or who currently smoke, should be screened for lung cancer,1 stigma and self-stigmatization often prevents these individuals getting screened. Another factor to consider is the heightened stress level that an individual experiences while awaiting screening results, whether it is in the short term or long term. “Interfacing with psychiatry and primary care doctors so [that these populations are] not missed,” is vital, she said.
Cognitive behavioral therapy and mindfulness interventions may be very helpful in managing patient stress, which can affect the quality of life of those individuals who are diagnosed with lung cancer and go on to treatment, Dr. Burgess said.
Dr. Burgess advised physicians and care staff to listen for patient distress to follow up regarding tobacco/smoking cessation if appropriate, and to refer if there are additional needs. Most of all, be aware of stigma and emotionally supportive throughout the entire process so patients know they are being heard.
Physical Function
Simon Ho, PT, DPT, CCS, of the University of Maryland delivered a presentation on malignant pleural mesothelioma (MPM), a rare incurable lung cancer linked to asbestos exposure.
Although overall survival from diagnosis tends to be 12-18 months for patients with MPM, better physical function, which is defined as the ability to perform tasks for daily living, is associated with shorter hospital stays, lower rates of surgical complications, and better rates of survival. Physical function in this population tends to be very limited, even before diagnosis, due to cardiovascular and pulmonary system involvement and pain.
Thus far, large studies of this patient population on physical function do not exist. Dr. Ho discussed data out of Japan that demonstrated that physical function was worse than baseline immediately after lung-sparing surgery but that it was improved and close to baseline by the 1-year post-operative.
Dr. Ho and colleagues conducted a retrospective study examining post-operative outcomes of lung-sparing surgery among 54 patients. They used the ECOG scale to measure limitations in physical function. ECOG scores predicted days spent on a ventilator (p = 0.01) and days in the hospital (p = 0.02). All patients were impaired in their physical function when they were released from the hospital, with older age being a predictor for impairment.
“We learned that physical function is predictive of important postoperative outcomes such as how long patients might be on a ventilator and hospital length of stay,” he said.
Dr. Ho noted that, going forward, combining both patient-reported outcomes and a physical test (e.g., walking and balance tests) would provide objective data and that early postoperative interventions are crucial.
“These findings demonstrate that we need to start rehabilitation early and throughout the continuum of care,” he said.
Qigong and Symptom Control
Complementary therapies are used alongside traditional cancer therapies to mitigate physical or emotional symptoms.
Shirley Siu Yin Ching, PhD, RN, of the Hong Kong Polytechnic University, delivered the results of a study combining Qigong, a form of exercise incorporating focused breathing and gentle movement, coupled with a meditation practice.
In a systematic review of 22 trials of Qigong, Dr. Ching concluded that this practice improved physical, mental well-being as well as quality of life in patients with various cancers, and she together with Prof. Molassiotis and Dr. Vu developed a study to see whether a cluster of the three most distressing lung cancer symptoms¬—dyspnea, fatigue, and anxiety—can be improved simultaneously.
The study recruited 156 patients with invasive lung cancer (mean age 57 years) from Vietnam who had completed chemotherapy or radiotherapy for at least 4 weeks.
The patients were divided into two groups:
- The intervention group participated in 90-minute supervised sessions of Qigong twice per week for the first 2 weeks and then were instructed to practice at home for 30-minute daily 5 times per week with DVD-led instruction. They were prescribed an additional 6-week follow-up practice (unsupervised).
- The waitlist control group was given the usual care with briefings on lung cancer care and a 10-minute meeting with a registered nurse.
The study demonstrated that the patients in the Qigong group reported a trend of improvement in the symptom cluster from baseline to 6 weeks (p = 0.002) and continued until 12 weeks (p = 0.015), whereas the control group did not experience a significant improvement. For fatigue and anxiety, the Qigong group showed a trend in improvement, and for dyspnea, there was a significant improvement over the control group. The Qigong group also had a significant improvement on the cough as well as self-reported quality of life.
Although the study did not support the hypothesis of alleviating dyspnea, fatigue, and anxiety as a cluster, it did improve dyspnea and cough significantly.
“In future studies, the cluster of symptoms that include dyspnea and cough should be considered as the key outcomes for Qigong intervention with breathing exercises,” Dr. Ching said, and the skill learned through the mindfulness-led breathing exercises should be investigated further.
Developing a Care Board
Professor Manuela Eicher, PhD, of the University of Lausanne and Lausanne University Hospital, in Switzerland, provided new insights into how interprofessional collaboration can benefit patients through a pilot program of a Care Board. In its initial pilot phase, it included a team of oncology nurses, oncologists, a palliative care physician, a social worker, a psycho-oncologist, a clinical nurse specialist in lung cancer, and a complementary medicine nurse or physician.
The aim was to meet twice per month to discuss the most complex cases in the lung cancer center. Once each patient’s most pressing needs were identified, the team would decide who be responsible to lead care provision at that moment. This group liaised with the tumor board to enable coordination with practical decisions about medical care.
“The oncologists were responsible to provide a direct link to the Tumor Board … to allow a direct link between these two boards,” Professor Manuela said.
The pilot sessions of the initial Care Board took approximately 50 minutes to discuss on average two patient cases. Top issues around supportive care included psychological needs, financial concerns, and a plan to introduce palliative care early into treatment.
The Care Board proved to be successful in communicating immediate needs and concerns of patients, as well as fulfilling those needs.
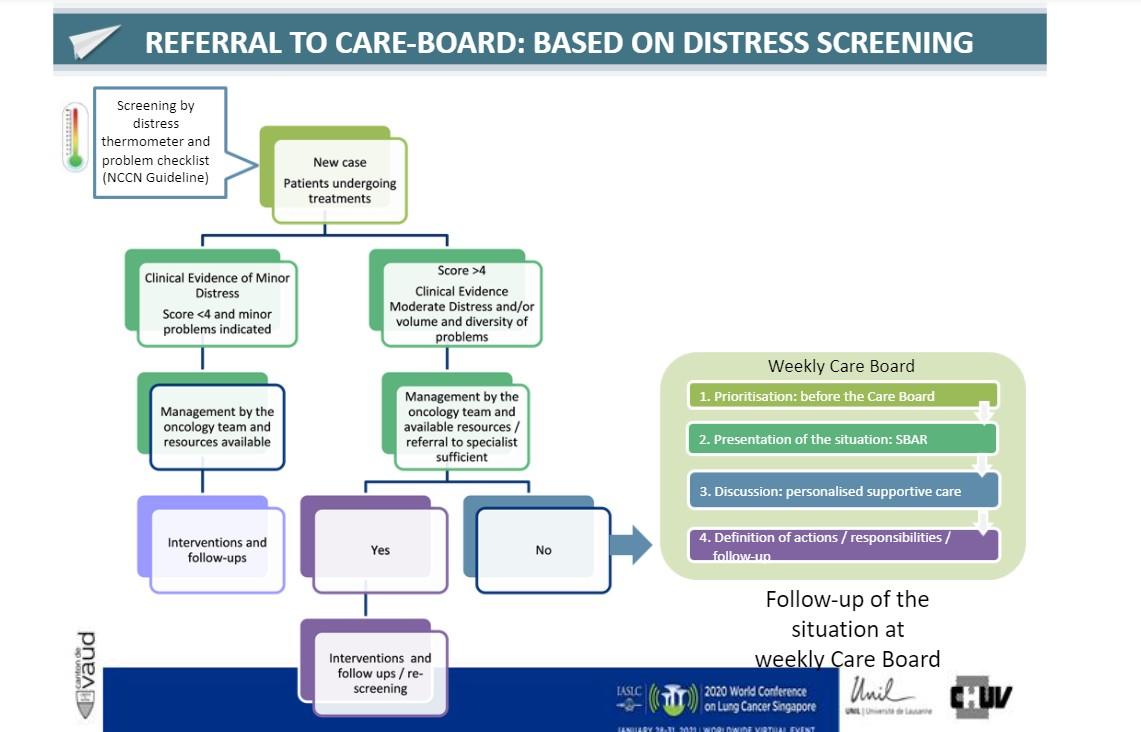
Going forward, some changes could be made to enhance the Care Board. It is now held weekly to enable more immediate action and open for other cancer patient populations. Inclusion criteria were better defined based on distress screening to enable a more structured discussion and prioritization (Figure).
The revised Care Board now includes nutrition experts and spiritual leaders to round out the physical and emotional needs of patients.
“Health care professionals described this as an opportunity to discuss and collaborate with physicians as equal partners. And all participants said that it enabled them to go beyond their field,” she said. “Early results show that the Care Board is feasible and accepted by health care professionals caring for [patients with] lung cancer. Early feasibility results for other patient groups are promising but need further research.”
This session had a real-time Q&A that provided attendees with the opportunity to ask questions of the session participants. The Q&As are included in the On-Demand recordings, available through the virtual platform. Registration is ongoing for the next 90 days at wclc2020.iaslc.org.
References:
- U.S. Preventive Services Task Force. U.S. Preventative Services Task Force Issues Draft Recommendation Statement on Screening for Lung Cancer. https://uspreventiveservicestaskforce.org/uspstf/sites/default/files/fi…. Accessed January 21, 2020.