Curative-intent resections for NSCLC often fail. Approximately 20% to 40% of patients with lung cancer who undergo curative-intent resection, experience a relapse, and die within 4 years. One key factor is the quality of the surgery, although there are no universal benchmarks of good quality resection, according to Raymond U. Osarogiagbon, MD, of the Thoracic Oncology Research Group, Baptist Cancer Center, Memphis. Dr. Osarogiagbon is a member of both the IASLC Membership and Staging and Prognostic Factors committees.
In his presentation during the mini oral, “MA03: New and Revisited Prognostic Factors in Early-Stage Lung Cancer,” Dr. Osarogiagbon said that the IASLC proposed a revised definition of complete resection for lung cancer that includes the quality of lymph node evaluation, beyond the status of the surgical resection margin. The current IASLC definition requires negative margins, systematic or lobe-specific nodal dissection, no extracapsular nodal invasion, and non-involvement of the highest mediastinal lymph nodes.
“Surgical quality deficits can induce unexpected imbalances in comparison populations, confounding discovery in non-small cell lung cancer, such as with adjuvant therapy and biomarker trials,” he said.
Evaluating Quality Markers
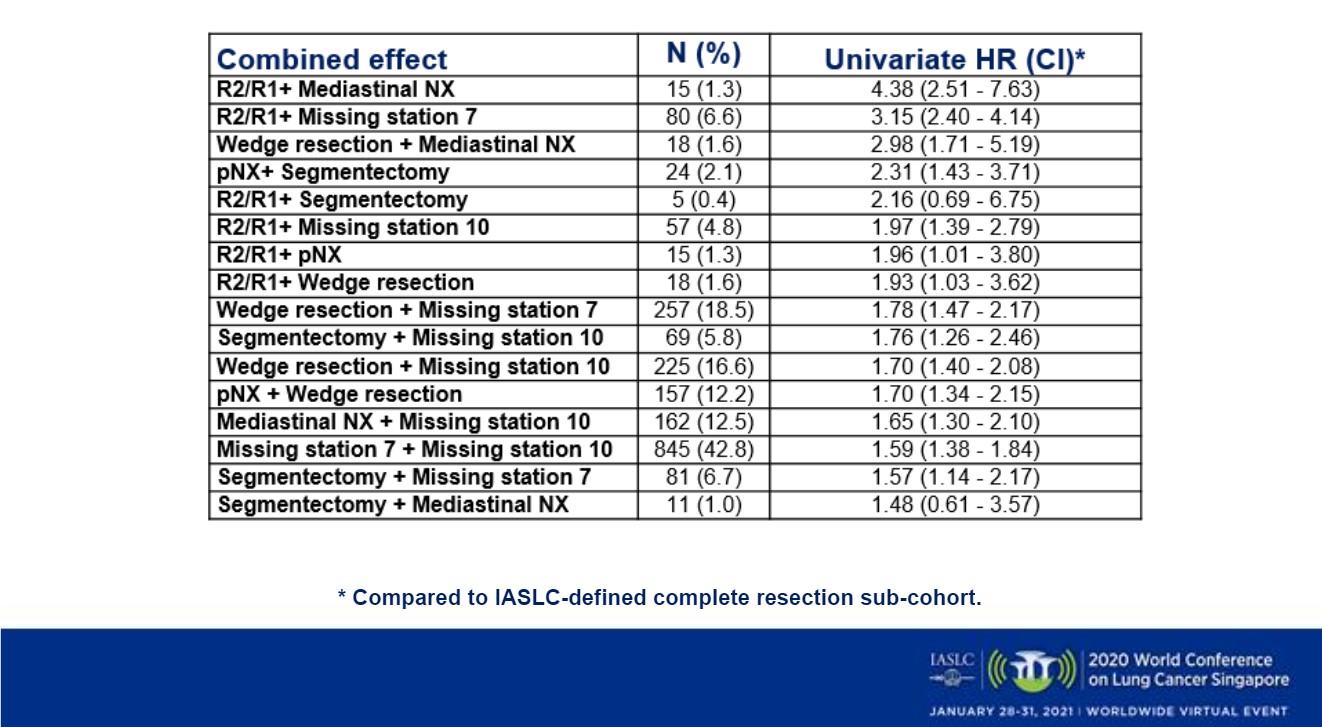
In a study of 12 hospitals between 2009 and 2012, his team evaluated the hierarchy of adverse surgical quality markers based on their individual and combined survival impact using the revised IASLC complete resection (CR) definition as a reference comparator. Benchmarks included extent of resection (i.e., wedge, segmental, lobar or greater), margin status (i.e., R0, R1, R2), and the examination status of specific lymph node stations such as hilar and mediastinal nodes.
Of 3,438 resections, 1,291 (33%) met the new IASLC-CR definition and served as the reference cohort. The cohorts with R1/R2 margin status had the worst outcomes. The other quality markers, noted below, had significantly worse-than-expected survival (Figure).
- R1/R2 HR = 2.60 (2.07 – 3.25)
- Wedge HR = 1.80 (1.39 – 2.32)
- pNX HR = 1.65 (1.34 – 2.04)
- pNXmed HR = 1.37 (1.12 – 1.67)
- Missing hilar station HR = 1.37 (1.11 – 1.69)
- Missing subcarinal station HR = 1.24 (1.07 -1.43)
These results led Dr. Osarogiagbon and his team to conclude this revised IASLC-CR definition is a practice-changing success, an improved method to evaluate the quality of surgery.
Discussant Wantao Fang, MD, Chief of Department of Thoracic Surgery at Shanghai Chest Hospital, also a member of both the IASLC and the Staging and Prognostic Factors committees discussed the presentation on the quality of surgery by Dr. Osarogiagbon.
Patients who underwent sublobular resections had worse than expected survival and suboptimal lymph node dissection, along with incomplete resection, which led the IASLC to re-evaluate their definition of a good quality resection.
Not included in Dr. Osarogiagbon’s study were factors such as whether the lesions were GGO-containing, as such lesions are known to be indolent and seldom have lymphatic involvement. Future studies should focus on whether different strategy on resection extent and lymph node management should apply to GGO-containing lesions.
Other prognostic factors being revisited by researchers include gender, or gender-related factors, such as smoking status and EGFR mutation status.
In addition, patients’ self-reported quality of life prior to surgery, including how much pain they are experiencing, is another predictor of post-surgical outcomes.
“Tumor characteristics as well as patient characteristics are important in predicting outcomes after treatment,” Dr. Fang said.
The management strategy should be modulated by prognostic factors, according to Dr. Fang.
This session had a real-time Q&A that provided attendees with the opportunity to ask questions of the session participants. The Q&As are included in the On-Demand recordings, available through the virtual platform. Registration is ongoing for the next 90 days at wclc2020.iaslc.org.