Treatment of operable, stage-I NSCLC with stereotactic ablative radiotherapy (SABR) was noninferior to video-assisted thoracic surgery (VATS) with mediastinal lymph node dissection (L-MLND).
Joseph Y. Chang, MD, of The University of Texas MD Anderson Cancer Center, presented the results of a single-arm trial comparing SABR with a published, longitudinally followed institutional cohort of patients treated with VATS L-MLND at the 2021 ASCO Annual Meeting (Abstract 8506).
With a median follow-up among the patients treated with SABR of 61 months, the 3-year OS rate was 91% with a 3-year PFS rate of 80%. At 5 years, the OS rate was 87%, and the PFS rate was 77%. According to the study protocol, noninferiority of SABR could be claimed if the 3-year OS was not lower than the historical VATS L-MLND (85.5%) by more than 12%.
In fact, the SABR arm was associated with significantly higher OS at 3 years (91% vs. 82%) and 5 years (87% vs. 72%) compared with VATS L-MLND (hazard ratio [HR]=0.441; 95% CI, 0.19-0.875; P = 0.021).
In his discussion of the data, Ramesh Rengan, MD, PhD, of University of Washington School of Medicine, pointed out that a study reported in 1995 established lobectomy with MLND as the standard of care for the management of operable early-stage NSCLC (LCSG 821). However, this approach is associated with morbidity as well as loss of functional lung, which has led to examination of less invasive alternative approaches.
Dr. Rengan said the results seen here were “excellent,” but added that other prospective and retrospective series that have endeavored to compare SABR with lobectomy in operable early-stage NSCLC have revealed a mixture of results, highlighting the challenges in performing these comparisons.
Study Details
The STARS study was originally designed as a phase III randomized trial comparing SABR with lobectomy but closed early due to slow accrual. Subsequently it was modified to a single-arm trial with historical comparative arm. Patients had to have histologically confirmed stage IA NSCLC.
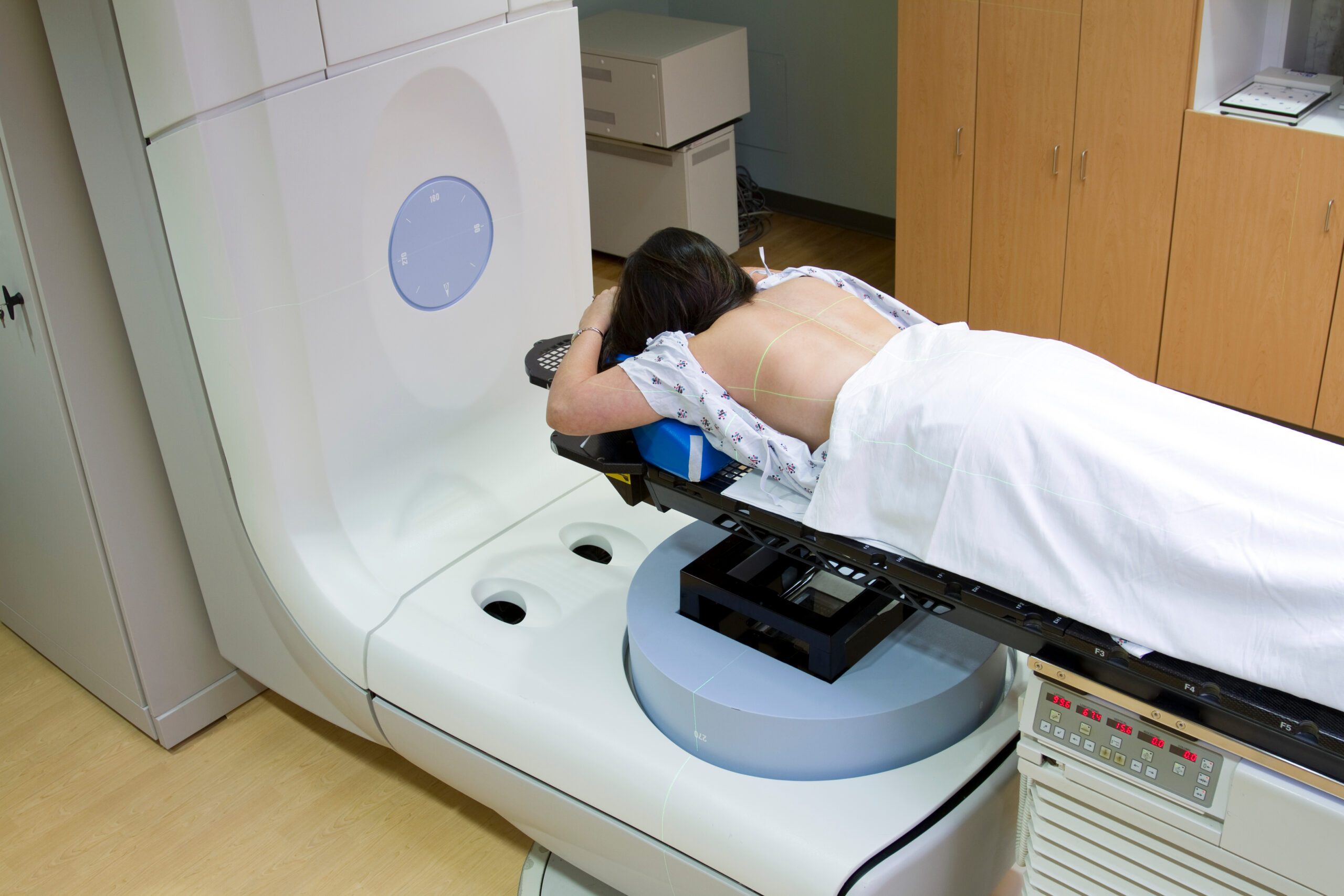
The patients received SABR utilizing 4-dimensional CT simulation and volumetric image guidance. Doses were 54 Gy in 3 fractions delivered to planning target volumes located peripherally or 50 Gy in 4 fractions to more central planning target volumes. Patients were followed by chest CT every 3 months for the first 2 years, every 6 months for another 3 years, and then annually.
Noninferiority was claimed for OS of SABR compared with VATS L-MLND.
Toxicities were minimal with no grade 4/5 toxicity. Two patients had grade 2 lung pneumonitis/fibrosis and one patient had grade 3 dyspnea. The 5-year cumulative incidence of secondary primary lung cancer occurred was 6.9%.
To minimize potential biases, propensity-matched comparisons were conducted with recent VATS L-MLND from the same period of STARS enrollment. In this analysis there was no difference in OS for 3-year survival (91% vs. 91%) or 5-year survival (87% vs. 84%) for SABR compared with VATS L-MLND (HR=0.78; 95% CI, 0.35-1.76; P =0.55). Again, noninferiority was claimed.
There was also no difference in cancer-specific survival, or local and distant failure rate. However, SABR was associated with a higher regional recurrence rate (12.5% vs. 2.7%). Chang noted that with the VATS procedure 10% of patients had lymph nodes upstaged at the time of surgical procedure and those patients received concurrent radiotherapy or radiotherapy. Among those patients, there were no regional recurrence, which may contribute to lower incidence of regional recurrence.
“Higher regional recurrence in SABR can be salvaged and doesn’t compromise OS and PFS,” Dr. Chang said.
There was no difference in PFS between SABR and VATS L-MLND at 3-years (80% vs. 88%) or 5-years (77% vs 80%; HR=1.29; 95% CI, 0.66-2.53; P = 0.46).
“SABR remains a promising approach for this population,” Dr. Chang said. “Multidisciplinary management is strongly recommended.”
Dr. Rengan agreed that the regimen discussed here may provide a more feasible alternative to the current standard for these patients. However, he also pointed out that from 1998 to 2021 after the report of LCSG 821 the rates of lobectomy use actually decreased from 55% to 50% of all early-stage NSCLC. Simultaneously, he said, the rates of SABR increased from 0% in 2003 to 6.6% in 2021 and the rates of sublobar resection also increased from 12% to 17%.
The ideal would be a prospective randomized clinical trial to compare SABR with VATS L-MLND; however, there have been four separate trials comparing SABR versus surgery in NSCLC that have failed to accrue or were deemed infeasible.
For the time being, Dr. Rengan said that lobectomy/MLND should continue to be considered the standard of care when feasible for early-stage NSCLC.
Reference:
Chang JY, et al. Stereotactic ablative radiotherapy in operable stage I NSCLC patients: long-term results of the expanded STARS clinical trial. Abstract 8506. Presented at: 2021 ASCO Annual Meeting.