It has been documented and accepted that lung cancer screening saves lives by detecting disease in high-risk individuals at earlier stages, making the disease more treatable and leading to improved survival and quality of life for these patients. Earlier treatment of disease also leads to exploration of new therapeutic models, which allows researchers and clinicians to begin to address other major health consequences from lung cancer and its treatments, such as elevated risk of cardiovascular disease.
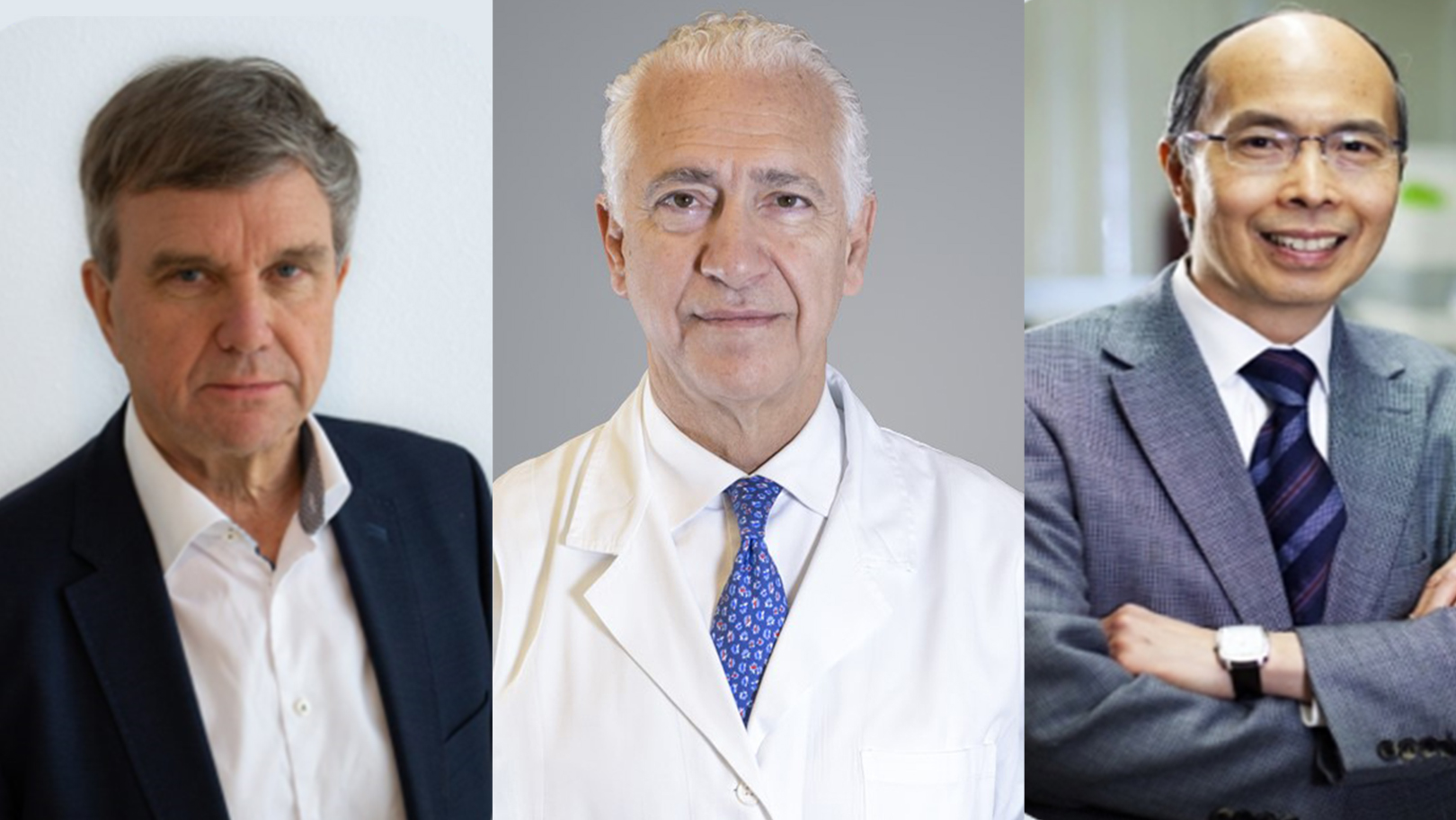
The CT Screening Symposium (CTSS), to be held May 7-8 virtually, will not only allow registrants to benefit from expert insights as to the logistics and rationale involved in implementation of a screening program but also will provide a focus on methodology, which, according to symposium Co-Chair Matthijs Oudkerk, MD, PhD, is the key to success.
“If you have well-defined recruitment with a good registry, quality control, follow-up monitoring, and data provision at set time points, you will get accurate and impressive results,” Dr. Oudkerk told CTSS News. “Now that we are on ‘step two’ of screening discussions in this type of conference environment—the first step being establishing whether screening actually impacts mortality and morbidity—we can start to influence standardization of screening on a global scale. This meeting is very important for everyone interested in lung cancer screening because we will be determining, by region, the methodology being used and its outcomes.”
COVID-19 and Screening
As with every other facet of life during the pandemic, the full impact of COVID-19 on lung cancer screening is unknown. However, it is obvious that numerous countries had reduced participation or even stopped screening altogether for a period of time. Because of this, it is expected that, globally, an increased number of lung cancer diagnoses will be made in the later stages of the disease. This could be true for the next several months or even years, depending on the duration of the pandemic in each region. However, symposium Co-Chair Stephen Lam, MD, wants to underscore that screening must and can continue through large-scale public-health crises.
“In lung cancer screening, we have the privileged position to be able to prioritize screening based on disease risk. We can screen the people at highest risk first and work our way down the list depending on screening capacity ” Dr. Lam said. “ A risk model-based approach in lung cancer screening is different from other cancer screening programs and uniquely suited to the type of global situation we are seeing with COVID-19.”
A Glimpse into the Future
Although this symposium’s presentations and discussions will be very much rooted in the current moment—definitions of and methodologies for screening programs across each region of the world—there will also be presentations on how to refine and evolve lung cancer screening.
Because each region’s population has specific features related to lung cancer incidence and potential management, looking across diverse populations will be key to both refinement of screening programs based on region and to developing standards ensuring that the needs of extremely diverse populations are met.
“We must take into account ambient air pollution exposures, and the area deprivation index, which is a ranking of regional socioeconomic disadvantages and access to healthcare into current risk-prediction models to improve accuracy of lung cancer risk assessment and achieve better equity across race and ethnicity,” Dr. Lam said.
In addition, tailoring screening based on both population- and individual-based factors could hone the accuracy of data, opening new doors into therapeutic research. Using risk-prediction models in conjunction with models based on the expected growth rate, screening programs can be more flexible as populations change. Through targeted screening, even individuals who have never smoked, could be assessed based on data illustrating the prevalence of genetic mutations that cause lung cancer in each region’s population.
Ugo Pastorino, MD, the third co-chair for the CTSS, has been passionate about targeted screening since well before COVID necessitated it. “Targeted screening involves not just tailored intervals based on level of risk but also a reduction of unnecessary radiation exposure from imaging studies, treatments, costs, and pain for patients. In addition, after twenty years of research, we can now reduce to a minimum level the risk unnecessary surgical resections for benign nodules or indolent disease, by active surveillance of non-solid pulmonary lesions,” he said.
Other forward-thinking approaches, such as use of artificial intelligence in the determination of an individual’s recommended screening intervals or in identification of more immediate actions such as physician follow up or even biopsy, also will be discussed formally and informally during the interactive live discussions.
“I expect that the next 5 years will show that the most impact in screening comes from the use of artificial intelligence,” Dr. Oudkerk said. “I think that we will be able to reduce the operator error maybe by as much as 70% over 5 years.”