The COVID-19 pandemic has had a devastating effect on lung cancer outcomes in the United Kingdom (UK). Fewer people have presented or have been referred for investigation, and those who do present have a more unfavorable stage. In October 2020, the Lung Cancer Coalition (UKLCC) published a report setting out a number of recommendations for mitigating the effect of the pandemic, both during the peaks and in the recovery and restoration periods.1 This report expands on recommendations by the UK Clinical Expert Group for Lung Cancer and Mesothelioma (UKCEG) published in March and June 20202,3 and the National Institute for Health and Care Excellence.4
The UKLCC report makes a slightly enigmatic statement that at least one-third of patients with lung cancer in the United Kingdom will have died over the 6-month period of the then-duration of the pandemic. This is derived from the Kaplan-Meier curve for lung cancer survival in the United Kingdom and assumes the same survival rate as before the pandemic and the same number of presentations over the 6-month period. However, the effect of the public messaging to “stay at home” has, in addition, led to a marked reduction in cancer referrals and evidence that fewer people are being diagnosed. This prompted another comment in the UKLCC report that suggested that some people with lung cancer will simply not have been recognized as having lung cancer, and that their deaths may even have been recorded as being related to COVID-19, especially prior to the implementation of widespread testing. Data are somewhat limited at present but suggest that the incidence of lung cancer has indeed fallen, again by at least one-third. Individuals may simply not be recognized by health services because they do not present or because they have difficulty accessing primary care. This is supported by the huge fall in diagnostic imaging and new-patient lung cancer attendances during the pandemic (Figure 1).5 Outside the pandemic, evidence from the United Kingdom from primary care electronic data show that where practices perform more chest X-rays, the number of people who have lung cancer detected is substantially greater.6 Furthermore, many of the people detected have a relatively short survival. Thus, the reduction in diagnostic imaging is likely to be a major contributor to the decline in incidence.
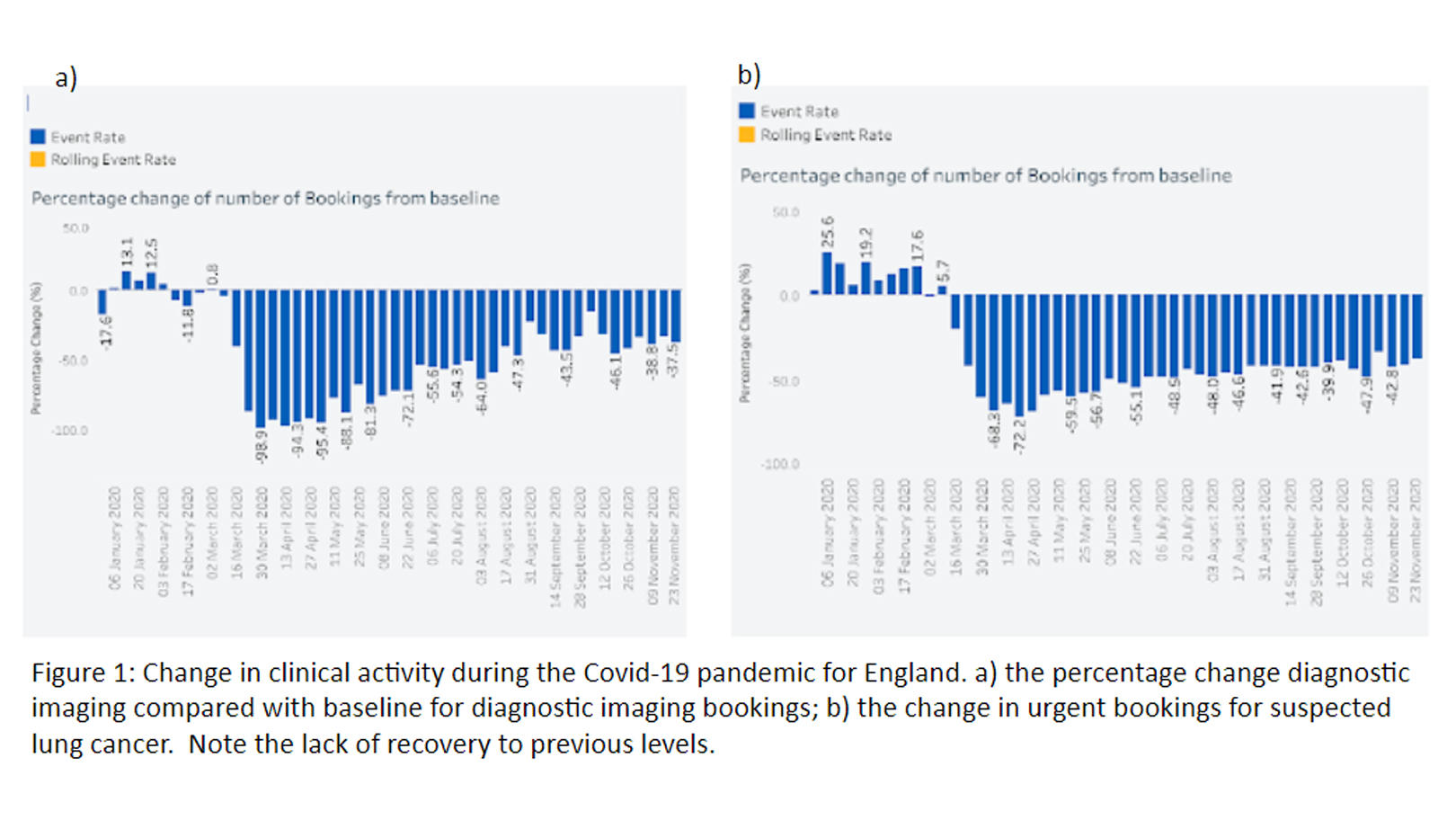
The fall in referrals for suspected cancer was most marked for lung cancer, presumably because of the overlap of symptoms between COVID-19 and lung cancer. The UKCEG attempted to mitigate this by producing guidance for primary care clinicians, “Differentiation of the Cs in lung cancer: cancer vs COVID.”7 The referral rates had only recovered modestly in the United Kingdom after the first wave, to around 65% of the expected figure; unlike breast cancer and colorectal cancers, there has not been an increase above the expected figure, signifying a degree of catch-up.5 This probably represents the rapidly lethal nature of lung cancer as well as the continued confusion that individuals may experience about symptoms that overlap with COVID-19 and some ongoing difficulties accessing advice.
Preliminary data from individual institutions in the United Kingdom show a shift toward later-stage disease, and this shift might be expected to be less marked because of the reduction in incidence of lung cancer such that people with later-stage disease have less chance of being diagnosed. Although these staging data are not yet mature and available for full analysis, it is clear to those clinicians working in lung cancer the effect that the pandemic has had: patients discussed at the multidisciplinary meetings now much more often have late-stage disease with relatively poor performance status. It is almost like working in lung cancer some 20 or 25 years ago. While this might be very disconcerting and frankly depressing for clinicians who care for patients with lung cancer, it does allow us to consider how we must redouble our successful approaches. In the United Kingdom and in other countries, there has been a major push toward the introduction of low-dose CT screening for lung cancer. This is likely to improve the outcomes considerably, although there are still concerns about cost-effectiveness in some countries. In the United Kingdom and other countries, there is also a problem with the speed with which patients present for services and progress to treatment. Several countries have developed nationally approved rapid diagnostic pathways (such as the National Optimal Lung Cancer Pathway in the United Kingdom8). These aim to accelerate the process so that the fall in performance status that many patients experience is minimized, enabling them to gain the maximum benefit from the excellent new treatments that are available.
Mitigation through Messaging
Many countries have also implemented awareness campaigns, including the United Kingdom. These can be associated with an improvement in the stage at presentation9 and show the power of public messaging (as indeed is the case with the COVID-19 pandemic, but in the wrong way in terms of its effect on stage at presentation).
It is evident that there is an urgent need to clarify the message to patients who may have symptoms suggestive of lung cancer, to mitigate the effect of further waves of the pandemic. Advice to clinicians is already available but needs to be widely implemented. The UKLCC report makes excellent recommendations, which would best be implemented alongside the urgent priority to control the pandemic and mitigate the incredibly damaging economic impact. Future research will establish the extent of the harm that the pandemic has done in the treatment of many diseases, and hopefully this research will show how we can improve the situation, should it occur again.
So far, the pandemic has justified many of the initiatives that have led to an improvement in lung cancer survival by showing what happens when they are halted. We should be clear that there should be immediate restoration of screening, awareness, and early and rapid diagnosis initiatives, and that they should be enhanced. Policymakers need to support this by ensuring that physical and human resources are in place to provide a workforce that can step up to the challenge, just as it has to that posed by the pandemic.
References:
- United Kingdom Lung Cancer Coallition. COVID-19 matters 2020. https://www.uklcc.org.uk/wp-content/uploads/2020/10/UKLCC-COVID-19-Matt…. Published October 2020. Accessed January 11, 2021.
- UK Clinical Expert Group for Lung Cancer and Mesothelioma. Recommendations for day case bronchoscopy services during the COVID-19 pandemic 2020. https://www.brit-thoracic.org.uk/document-library/quality-improvement/C…. Published May 11, 2020. Accessed January 11, 2021.
- UK Clinical Expert Group for Lung Cancer and Mesothelioma. Lung cancer and mesothelioma service guidance during the COVID-19 pandemic 2020. https://www.brit-thoracic.org.uk/document-library/quality-improvement/C…. Published July 15, 2020. Accessed January 11, 2021.
- National Institute for Health and Care Excellence. COVID-19 rapid guideline: delivery of systemic anticancer treatments 2020. https://www.nice.org.uk/guidance/ng161. Published March 20, 2020. Updated November 9, 2020. Accessed January 11, 2021.
- NHS Digital. NHS e-Referral Service (e-RS) open data dashboard 2021. https://digital.nhs.uk/dashboards/ers-open-data. Updated November 25, 2020. Accessed January 11, 2021.
- O’Dowd EL, McKeever TM, Baldwin DR, et al. What characteristics of primary care and patients are associated with early death in patients with lung cancer in the UK? Thorax. 2015;70(2):161-168.
- UK Clinical Expert Group for Lung Cancer and Mesothelioma. Differentiation of the Cs in lung cancer: cancer vs. COVID 2020. https://www.brit-thoracic.org.uk/document-library/quality-improvement/C…. Published November 29, 2020. Accessed January 11, 2021.
- NHSE CEGfLc. National Optimal Lung Cancer Pathway 2017. http://content.smallerearthtech.co.uk/system/file_uploads/16086/origina…. Published August 2017. Reviewed May 2019. Accessed January 11, 2021.
- Kennedy MPT, Cheyne L, Darby M, et al. Lung cancer stage-shift following a symptom awareness campaign. Thorax. 2018;73(12):1128-1136.