Two studies presented at the WCLC Congress 2021 include data that suggest the potential need to update the current TNM classification of lung cancers by implementing additional pathological elements to the evaluation of the specimen.
Commenting on these two studies, Jorge Alatorre-Alexander, MD, of Instituto Nacional de Enfermedades Respiratorias, Mexico City, Mexico, admitted that reclassifying tumors from the 7th Edition of the UICC/AJCC to the 8th Edition was not easy and required a lot of work to try to better understand the behavior of these tumors.
“Things will need to be done even better for the next edition,” Dr. Alatorre-Alexander said. “By 2021, we understand that the TNM is the most important prognostic tool we have, but there are also other factors of prognostic interest.”
These include things like patterns/grade and pleural invasion.
Results of the first study, presented by Pietro Bertoglio, MD, of IRCCS Azienda Ospedaliero Universitaria di Bologna, Italy, looked at the effect of patterns and grade NSCLC. The data suggested that T1a-b-c lung adenocarcinoma presenting a high-grade pattern should be upgraded to T2a. Integration of these histological features in the TNM could better stratify patients according to their risk of recurrence, Dr. Bertoglio and colleagues suggested.
“We all know that the presence of high-grade adenocarcinoma patterns is related to worse long-term outcomes,” Dr. Bertoglio said. “The current TNM is only based on anatomical and microscopic features while histological and molecular characteristic are not taken into account, currently.”
High-grade Patterns
In the retrospective study, Dr. Bertoglio and colleagues wanted to verify the possible effect of high-grade patterns on the T factor of the TNM and its possible influence on stage. They used data of 607 consecutive patients with resected pT1-T3N0 lung adenocarcinoma from nine European thoracic surgery centers. All patients were staged according to the 8th Edition of TNM.
More than one-third of patients (37.9%) had at least one high-grade component, of which 169 were solid and 75 were micropapillary. The researchers stratified patients by their T component and the presence of high-grade patterns and found that T1a-b-c high-grade and T2a non-high-grade patterns were significant prognostic factors (P = 0.002 and P = 0.034, respectively).
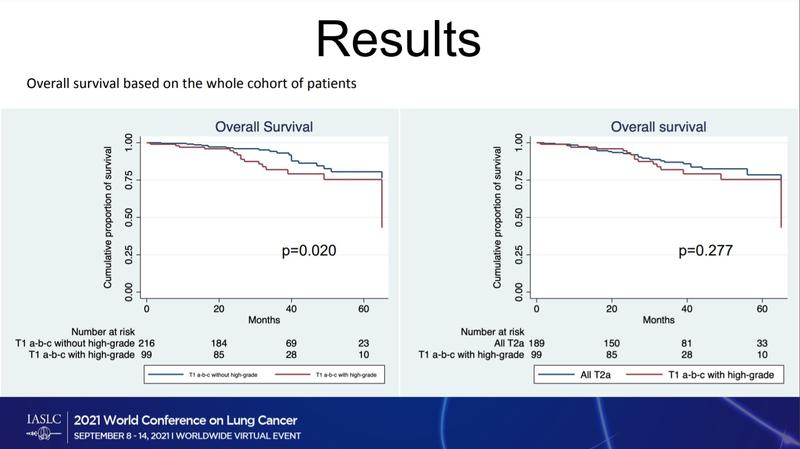
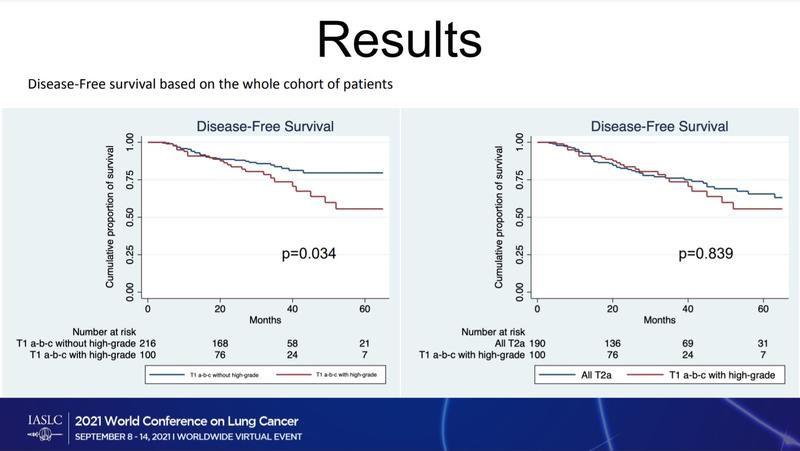
There was a significant difference in overall survival (OS) for T1a-b-c without high-grade component compared with T1a-b-c with high-grade component (P = 0.020). However, there was no difference in OS for all T2a tumors and T1a-b-c with high-grade components.
T1a-b-c with no high-grade component had significantly better disease-free survival (DFS) than T1a-b-c with high-grade pattern (P = 0.034). Again, there was no difference in DFS for T2a tumors and T1a-b-c with high-grade components. Multivariate analysis confirmed that pathological T component were significant prognostic factors for OS (HR = 1.088; 95% CI: 1.005-1.177; P = 0.037) and DFS (HR = 1.123; 95% CI: 1.059-1.192).
In his discussion of the results, Dr. Alatorre-Alexander noted that the magnitude of the effect seen in the multivariable analysis may not be large enough to make it clinically meaningful or to consider that upstaging will be needed.
To validate the data, the researchers also performed a propensity score matched analysis using gender, age, surgical approach and pT factor as variables; 230 matched pairs were included. This analysis confirmed that T1 patients with no high-grade patterns had significantly better overall survival and DFS compared with T1 with high-grade pattern.
“Adenocarcinoma histological grade had a significant influence on OS and DFS,” Dr. Bertoglio said. “We propose that the use of the presence of adenocarcinoma high-grade component in T description might better stratify patients and define risk categories.”
Commenting on the study, Paul Van Schil, MD, PhD, of the department of Thoracic and Vascular Surgery, Antwerp University Hospital, Belgium, said the finding that a high-grade category comprising micropapillary and solid adenocarcinomas were negative prognostics factors is also recognized in the recently published 5th edition of the World Health Organization’s classification of thoracic tumors, “making a distinction between well-differentiated, moderately differentiated, and poorly differentiated invasive adenocarcinomas.”
The IASLC is currently encouraging its members and other thoracic oncology professionals to submit patient data like that in this study to better inform the 9th Edition of the TNM Classification for Thoracic Cancer. Included patients must have bene diagnosed with lung cancer between January 1, 2011 and December 31, 2019 or mesothelioma between July 1, 2013 and December 31, 2020.
“When more data from the prospective IASLC database become available in 2022-2023, the high-grade pattern may be incorporated in the newly proposed TNMX system, which comprises classical anatomical (TNM) and non-anatomical (X) prognostic factors,” Dr. Van Schil said.
Pleural Invasion
The second study examined pleural invasion (PL) PL1/PL2 involvement in patients with T2 NSCLC. Ismail Sarbay, MD, thoracic surgery resident from Istanbul University-Cerrahpasa Cerrahpasa Medical School, Istanbul, Turkey, presented the results.
“The invasive characteristics of tumors are considered as prognostic factors; therefore, staging systems are adding or adjusting T factors according to invasion,” Dr. Sarbay said. “The latest TNM staging system accepts invasion from tumor to pleura, vessels, mediastinum, etc., as prognostic factors in addition to tumor size. Presence of visceral pleural invasion or PL upstages the tumor with a diameter below 3 cm as T2.”
The study looked at 804 patients who underwent resectional surgery for NSCLC between 2003 and 2019. Of these, 25.2% were considered to have T2 tumor. PL1-2 was reported in 65% of patients (Group 1) and no pleural invasion in 35.0% of patients (Group 2).
The median follow-up was 38 months. The groups were balanced for age and gender. Male gender had significantly lower survival in both groups compared with female (mean 132 vs. 162 months; P = 0.05). A multivariate analysis showed that gender, age, and PL status were independently associated with survival.
Patients with PL1/PL2 tumors had a mean 122-month survival time compared with 159 months for patients with PL0 T2 tumors (P = 0.016). N factor and the presence of PL1/PL2 were independently associated with survival (P = 0.04 and P = 0.03, respectively).
“Previous studies and guidelines describe PL as a prognostic factor, which is worth considering when staging a tumor,” Dr. Sarbay said. “Our study showed PL status independently worsened survival in T2 patients; therefore, we are suggesting PL1/2 status should be considered as a new subgroup in T2, such as T2c.”
In his discussion, Dr. Alatorre-Alexander said that it is known that visceral invasion is a well-known prognostic factor, but that there are other T2 factors that are also known to confer worse prognosis. He doubted that any of these factors warrant reclassification of these tumors.
According to Dr. Van Schil, these data did show that visceral pleural involvement by a NSCLC is another negative prognostic factor. Also in this study, nodal involvement and PL1/PL2 status were found to be independent, negative prognostic factors.
“Whether patients with T2 NSCLC should be upgraded to a new category T2c as the authors propose, or even T3, requires additional, prospectively collected data with adequate follow-up in a larger number of patients,” Dr. Van Schil said.
As clinicians await the publication of the 9th edition of TNM guidelines, it will be interested to see how new molecular information is incorporated into tumor classification, Dr. Alatorre-Alexander said.
“I appreciate the effort of all of my colleagues in contributing to the improvement of knowledge for a better understanding of this disease,” he said.